不锈钢、钛合金和钴铬合金等医用金属材料因其优越的力学性能、界面稳定性和良好的生物相容性,广泛应用于骨科及血管介入等植入性医疗器械[1,2]。然而,除了人工关节、脊柱内固定植入物等人体承重部位的器械需要提供永久支撑外,大多数时候人体对于植入物提供的支撑、固定等功能的需求只是暂时的。植入物长期存留体内还会带来不可预期的负面影响,例如骨折的病人再次骨折的风险增加1.4~2.5倍,其中重要的因素就是骨折内固定用的不锈钢板和螺钉与人体骨因弹性模量的巨大差异造成应力遮挡而引起骨质流失[3,4];约10%的患者支架术后存在内皮愈合不良或功能障碍导致的血管再狭窄和血栓,其原因即永久存在的支架平台对血管的持续刺激[5,6]。此外,永久支架相当于给血管套了“金属夹克(metal jacket)”,使血管舒张受限,特别是禁锢婴儿或儿童正在生长的血管[7,8]。锌合金是和镁合金、铁合金共同受到关注的一类可降解金属。由于其腐蚀速率介于镁合金与铁合金之间,具有较为理想的降解行为,成为近年来的研究热点[9,10]。Mg、Fe、Zn的性质见表1[11~15]。近年来,研究者对锌合金的设计、加工制备以及降解机理进行了大量的研究,但对其体内外生物相容性的研究尚不充分,仅评估了体外细胞毒性、溶血、凝血,只有少数材料植入动物体内进行了组织相容性的表征。然而锌合金器械在植入体内后,会引起一系列复杂的机体反应,同时机体生理活动中的力学运动、生物化学作用和生物电、磁场等作用会以各种形式影响其力学性能和降解行为,随着材料的降解和力学性能的丢失,可能对机体的组织或器官产生复杂而长期的影响。因此系统、全面的生物相容性评价关系着锌合金器械临床应用的安全性和有效性。
| Metal | Standard electrode | Yield | Young's | Shear | Elastic | Hardness | Required | Develop |
|---|---|---|---|---|---|---|---|---|
| potential | strength | modulus | modulus | modulus | HV | element | -ability | |
| V | MPa | GPa | GPa | GPa | ||||
| Mg | -2.37 | 51-244 | 44-45.5 | 16-18 | 44-48 | 38 | Yes | No |
| Zn | -0.76 | 285-325 | 90-110 | 35-45 | 14-32 | 42 | Yes | Yes |
| Fe | -0.44 | 108-122 | 204-212 | 78-84 | 195-235 | 157 | Yes | Yes |
1 医用锌合金材料化学成分和物相组成分析
由于合金元素含量一般比较低,Zn(OH)2、ZnO、Zn3(PO4)2和ZnCO3是降解过程中的主要产物[21,22]。表2列出了锌合金主要降解产物的物理化学和毒理学性质。Zn(OH)2是锌合金降解的中间产物,常与ZnCO3共价结合ZnCO3·3Zn(OH)2。ZnO微溶于水,具有收敛性和抗菌能力,也是常用的营养增补剂。ZnCO3·3Zn(OH)2不溶于水,也无毒。相对于ZnO和Zn(OH)2,Zn3(PO4)2可溶于水,更容易被机体转运、吸收。一个锌支架大约50 mg,以全部转化为Zn2+计算,远低于导致全身毒性的安全阈值(ZnCl2的半数致死量约为500 g/人)。此外,Zn是人体必需的微量金属元素,组织分布广泛,锌合金植入物游离出来的锌离子可能还会参与维持机体生理功能和正常代谢[23]。人体内至少300种酶以Zn为辅助因子参与糖类、脂质、蛋白质和核酸代谢[24,25]。从DNA甲基化的表观遗传变化到发育,癌症进展/抑制,骨骼重塑/矿化和动脉粥样硬化,Zn在预防和治疗各种病理状况中起着关键作用[26,27]。Hennig等[28]的综述文章表明,Zn具有很强的抗动脉粥样硬化特性,作者认为,这种行为源于锌离子作为抗氧化剂和内皮细胞膜稳定剂的作用。另外,Zn也是骨骼形成和矿化必需的元素,能够刺激成骨细胞生长,同时抑制破骨细胞行使骨吸收的功能[29]。在大脑中,Zn可通过谷氨酸能神经元储存在特定的突触囊泡中,调节大脑的兴奋性,对大脑和中枢神经正常功能的发挥起着至关重要的作用[30,31]。Zn的组织分布和功能多样性为锌合金的临床应用提供了先决条件。锌合金的加工过程及其降解产物的性质表明了锌合金在人体中的应用具备基本的安全性,可以用来制做血管支架、腔道支架、软组织闭合和伤口修复、骨修复产品(夹、钉)等[32~35]。
表2 锌合金主要降解产物的性质
Table 2
| Degradation | Solubility, 20oC | Stability | Density | LD50, acute systemic | Equivalent to human | Toxicity |
|---|---|---|---|---|---|---|
| product | g·L-1 | g·cm-3 | toxicity, oral, rat | lethal dose | level | |
| mg·kg-1 | g | |||||
| ZnO | 0.0029, | Stable | 5.68 | > 2000 | 50 | Low toxicity |
| slightly soluble | ||||||
| ZnCO3·3Zn(OH)2 | Insoluble | Stable | - | > 10000 | 500 | Non-toxic |
| Zn3(PO4)2 | 2.7, | Stable | - | > 5000 | 500 | Non-toxic |
| slightly soluble | ||||||
| ZnCl2 | Soluble | Stable | 1.01 | > 5000 | 500 | Non-toxic |
2 生物相容性评价方法
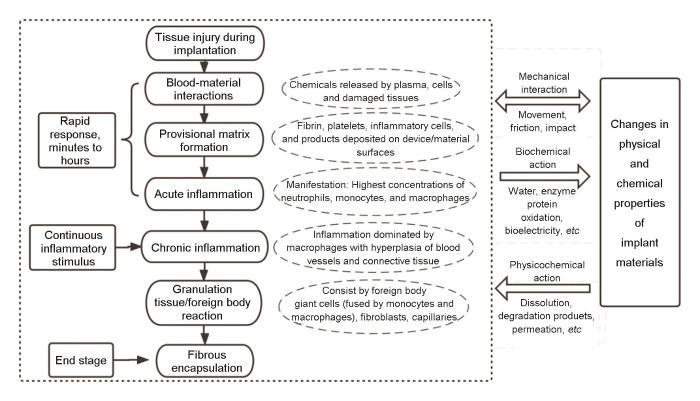
图1
2.1 生物相容性影响因素
影响医疗器械生物相容性的因素主要有:(1) 材料物理化学、形态学和表面特性表征;(2) 工艺过程中预期的添加剂,产生的工艺污染物和残留物;(3) 可沥滤物质;(4) 不同组件间的相互作用;(5) 终产品的性能与特点。器械中相关原材料、工艺污染物、可沥滤物的化学特性与生物相容性关系最为紧密,其与组织的接触性质、程度、频率和持续时间极大影响机体的反应[40]。有证据表明,一些金属元素,特别是Ni,可以刺激免疫系统,在包括过敏反应和炎症反应在内的不同病理的发生中发挥作用[41,42]。接受含Ni血管内支架的患者发生再狭窄一定程度上跟镍过敏有关[43,44]。除此之外,物理特性对器械的生物相容性也有较大影响,如多孔材料的孔径尺寸和孔隙率影响组织细胞的黏附、生长[45,46],磨损的颗粒尺寸和形状影响局部组织的炎症反应程度[47,48]。材料表面的拓扑结构如表面粗糙度、曲率及规则的几何图案影响蛋白质的黏附、细胞的增殖及形成血流的扰动[49,50]。血浆中的凝血因子蛋白在血液接触器件表面的快速吸附和激活是诱发血栓生成的主要途径[51,52]。值得注意的是,降解产物及周期影响植入物与人体的动态反应,一些可降解止血材料(如淀粉多糖、壳聚糖、再生氧化纤维素等)相较于非降解材料(如高密度聚乙烯)往往在植入试验中表现出程度更高、周期更长的炎症反应[53,54]。
2.2 生物学评价方法
目前我国对拟上市医疗器械的生物学评价采用GB/T 16886标准,该系列标准等同采用ISO 10993国际标准。根据GB/T 16886.1—2022 《医疗器械生物学评价 第一部分:风险管理过程中的评价与试验》对医疗器械按临床使用部位和接触时间分类,以选择合适的生物学试验项目。
表3列出了医用锌合金器械需考虑的必要生物学试验项目。对于医用锌合金制作的可降解的植入组织/骨的医疗器械,一般选取细胞毒性、皮肤刺激、迟发型超敏反应、急性全身毒性反应、(亚)慢性全身毒性反应、遗传毒性、植入后局部反应和降解。表4列出了需考虑的补充试验项目。例如,如果用于制造接触循环血液的支架,应增加血液学评价;如果用于制造宫内节育器、子宫托等与生殖系统有关的医疗器械,应增加生殖发育毒性的相关试验。理论上,还应考虑进行毒代动力学试验,但其必要性应结合器械/材料的预期用途,终产品化学组分,降解产物及可沥滤物(参照GB/T 16886.16—2021)。以支架为例,切割抛光好的锌支架重量大概50 mg,以全部是Zn元素计算,假设在1 a内完全降解,预期的每日剂量为140 μg,仅是成年男性推荐每日摄入量15 mg的1%。因此锌支架的植入并不会影响机体的血液系统、神经系统、消化系统、免疫系统等,如果锌支架在原位的降解过程没有引发强烈的炎症和过敏反应,即可认为无需进行毒代动力学的研究。同样的,只有当来自其他来源的数据表明有肿瘤诱导的倾向时,才应进行致癌性试验(参照GB/T16886.3—2019)。致癌性试验没有规定的标准和方法,可在动物试验中观察和记录原位组织和易感组织的肿瘤生成情况。
表3 锌合金植入器械必要的生物学试验项目
Table 3
| Test item | Current standard | Purpose and method | Judgement criterion | |
|---|---|---|---|---|
Cellular response | Cell toxicity | GB/ T16886.5—2017 | The device/extract was cultured with cells, its potential cytotoxicity was evaluated by morphology and metabolic activity, such as MTT method | Cell viability > 70% was considered non-cytotoxic. For Zn-based materials, it is generally necessary to dilute the extract over a range of concentrations. Evaluate the result in vitro and in vivo comprehensively |
Tissue response | Intradermal reaction | GB/T16886.10—2017 | Intradermal injection of devices/materials extracts on the back skin of rabbits, to evaluate the non-specific percutaneous acute irritant effects of leachables | Erythema, edema, eschar, etc., were observed and scored according to the standard. The difference between the average scores of the test sample and the control should not be greater than 1.0 |
Implantation & degradation | GB/ T16886.6—2015 | Final devices/materials are implanted by surgical or interventional operation, and the target tissues are collected and observed at different time points to evaluate the local toxic effect of the sample on the living tissue and the degradation process (product) | Different degrees of tissue reactions (aseptic inflammation, fibrous cysts around the implant, etc.) will appear after implantion. With the influence of degradation, the reaction is higher and longer relatively. It's best to set a similar marketed product control | |
Immune response | Delayed type hypersensitivity | GB/T16886.10—2017 | The immunity is usually induced by injecting the extract of the device/material plus protein to guinea pigs, and stimulated again after 2 weeks. Then the skin reaction is observed to evaluate the potential contact sensitization of the sample | No local skin erythema, edema and other inflammatory manifestations was considered to be no delayed type hypersensitivity reaction. Allergic reactions do not limit its use necessarily |
Systemic response | Acute systemic toxicity | GB/T16886.11—2011 | Mouse is used routinely. Intravenous and intraperitoneal injection of the device/material extract is contacted with animals. The systemic response is observed to evaluate whether the sample releases toxic substances and produces acute systemic toxicity. The maximum exposure dose is 50 mL·kg-1 body weight | Clinical performance (coat, skin, mucous membranes, respiration, muscles, behavior, etc.) should be observed and no indications. Gross pathological evaluation should be considered if clinically indicated |
(Sub)chronic systemic toxicity | Rat is used routinely. The devices/materials or extracts are (repeatedly) contacted with animals by appropriate routes such as implantation, intravenous or intraperitoneal injection. The dose range is determined according to human safety limits. Clinical manifestations, body weight changes, hematological and clinical biochemical indicators, clinical pathological, gross pathological and histopathological analysis, etc., to evaluate whether the long-term exposure of sample to the human body will release toxic substances and produce (sub)chronic systemic toxicity | Compared with the control group, no significant difference should be observed in each index | ||
Blood system | Hemolysis | GB/ T16886.4—2003 | Direct contact of blood with the device/material or its extract, measuring the amount of hemoglobin released by erythrocytes to evaluate the degree of erythrocytelysis and hemoglobin release caused by the device/material | Hemolysis rate should be < 5% |
Genetic system | Genotoxicity | GB/ T16886.3—2019 | Mammalian or non-mammalian cells, bacteria, yeast or fungi are used to determine whether a device/material or extract causes genetic mutations, changes in chromosome structure and number, or other changes in DNA or genes. Bacterial gene mutation, chromosomal aberration and mouse lymphoma test are the most used in vitro tests | There should be no significant difference compared to the negative control. If the in vitro test cannot be carried out or the results are confusing, further in vivo chromosome analysis and micronucleus test of mammalian bone marrow cells should be used |
表4 锌合金植入器械补充的生物学试验项目
Table 4
| Test item | Current standard | Purpose and method | Judgement criterion | |
|---|---|---|---|---|
Blood system | Coagulation | GB/ T16886.4—2003 | The devices/materials are directly contacted with venous blood and poor platelet plasma (usually rabbits), respectively, and the clotting time is measured to evaluate whether the sample contains endogenous coagulation system activators | Specify the acceptable criteria of the device/material on a verifiable basis (eg, compared to an approved device of the same type) |
Platelet adhesion | The device/material is co-cultured with fresh sodium citrate anticoagulated whole blood (human, sheep or rabbit, etc.). The platelet adhesion on the surface of sample is observed to evaluate the effect of the sample on platelet performance | |||
Thrombosis | The device/material is implanted into the vein. Thrombus formation on the surface of the sample and the intima surface of the blood vessel are observed and scored to evaluate the potential of forming thrombosis | |||
Complement system | The device/material is contacted with human serum, and the concentration of C3a fragment formed during complement system activation is assessed by enzyme-linked immunosorbent assay to evaluate the effect of the sample on complement activation | |||
Reproductive system | Reproductive toxicity | GB/ T16886.3—2019 | 8-10 weeks before mating, male and female animals (mouse) are continuously exposed to device/material or extracts until 21 d after the birth of F1 generation. The sexual function, estrus cycle, mating behavior, conception, parturition, lactation, and weaning of animals as well as the growth, development, deformity, morbidity and mortality of offspring are observed and recorded, to evaluate the influence of the sample on the reproductive function and embryonic development | There should be no significant difference compared to the negative control |
Metabolic system | Toxicokinetics | GB/T16886.16—2021 | To study the quantitative changes in the process of absorption, distribution, metabolism and excretion of the test substance in the body, degradation products, leachables, and metabolites of device/material should be qualitatively detected and quantitatively analyzed. Rodent models (rats, mice) are generally used. Blood, urine, feces and bile are collected regularly after exposure, and the heart, liver, spleen, stomach, kidney, gastrointestinal tract, gonads, brain, body fat, skeletal muscle and other tissues are collected, respectively, to determine the distribution of the test substance. Bioavailability, toxicity-time curve, apparent volume of distribution, clearance rate, half-life, average residence time, maximum and maximum concentration (time) of the test substance were measured through the toxicokinetic model | The mathematical model expression of metabolic process, combing with the physical and chemical shape, administration route, dose and method of the test substance is evaluated comprehensively |
医疗器械生物学试验的方法大多源自药物或化妆品的毒理学方法,样品制备方法也是针对不可降解材料,通过浸提的方法提取产品中的可沥滤物、加工助剂等可能影响产品生物相容性的物质。浸提过程受温度、时间、浸提介质(极性、非极性)、浸提比例以及材料的相平衡影响,因此GB/T 16886.12—2017对浸提液制备条件和方法进行了具体规定。由于锌合金在体内外降解行为的差异以及复杂的临床应用场景(血管支架、腔道支架、骨钉骨板、吻合钉、宫内节育器等),为避免受到不必要的限制或产生虚假的安全感,因此尚无针对该类产品的标准浸提液制备方法。当采用浸提液进行体内试验(如致敏、皮内反应、全身毒性、遗传毒性等)时,如浸提液中出现颗粒物无法直接用于试验,可考虑采用过滤、离心等方式去除,但应通过电感耦合等离子体发射光谱(ICP-OES)或电感耦合等离子体质谱(ICP-MS)等手段分析处理前后的元素组成和浓度,并进行方法学论证(参照GB/T 13748.15—2013)。如浸提原液具有细胞毒性,应分析其原因并对浸提原液进行梯度稀释(至无细胞毒性),再结合体内试验中植入物附近降解产物大量释放或积聚时对局部细胞活性及局部组织炎症反应的影响,对产品的生物安全性进行综合评价(参照GB/T 16886.15—2003)。
3 锌合金生物相容性研究现状
生物相容性评价最终以产品为导向,但目前锌合金植入器械只有用于颌面修复的骨板骨钉和心血管支架走到了临床试验阶段,未见其他产品报道进展。因此本文通过锌合金材料的生物相容性分析研究进展和未来的方向。
3.1 细胞毒性研究
细胞是发挥生物体功能的基本单位,细胞毒性是生物学试验中的首选项目,可为其他生物学危险源的识别和评估提供初步证据[55]。对于可降解医用金属器械/材料,细胞毒性主要受以下方面影响:金属表面性质如形貌、表面能、离子释放浓度、降解产物以及局部微环境(如pH值)变化[56~58]。其中,对细胞毒性影响最大的是离子浓度。根据对人体的作用分为有益金属离子(如钙、镁、铁、锌等离子)和有害金属离子(如汞、铬等离子)。即使是有益的金属离子,与人体的关系仍然存在剂量效应,当浓度太高时,也会因阻碍其他有益金属的结合而产生毒性。Ma等[59]研究了人主动脉内皮细胞(HAEC)在不同浓度(0~140 μmol/L) Zn2+环境中的短期细胞反应。低浓度Zn2+可使细胞活力、增殖、黏附、扩散和迁移能力增强,同时降低细胞黏附强度。然而,较高浓度Zn2+ (> 100 μmol/L)对HAEC行为表现出相反的影响(抑制细胞活力、增殖、迁移等)。Shearier等[60]研究显示,人体细胞对Zn2+的耐受性:HAEC (半数致死量LD50:265 μmol/L) > 平滑肌细胞(AoSMC) (LD50:70 μmol/L) > 真皮成纤维细胞(HDF) (LD50:50 μmol/L)。Kubasek等[61]研究表明,Zn2+对人骨肉瘤细胞(U-2 OS)和鼠成纤维细胞(L929)最大安全浓度分别为120和80 μmol/L。研究者们普遍认为不同的细胞品系针对锌合金材料会表现出不同的细胞反应,大概是由于不同类型的细胞尺寸、形态、细胞膜的转运过程、行使的功能以及细胞所处的微环境存在差异。这提示不同的可降解锌合金材料可能有其最佳应用场景,比如某一类材料更适合做骨科植入物、血管支架、腔道支架甚至宫内节育器。
在同一种应用场景下,有哪些措施可以改善锌合金器械/材料的细胞相容性呢? (1) 制备锌合金保护膜涂层。Shearier等[60]在金属Zn片上直接培养HAEC、AoSMC和HDF细胞,发现活细胞的数量几乎可以忽略不计。胶原蛋白和明胶表面修饰过的Zn片上,以上细胞均可附着和增殖。Jablonska等[62]在模拟体液(SBF)中预孵育Zn-1.5Mg合金,在表面形成保护性膜层,也可以减少离子释放量并增强初始细胞黏附。(2)添加适宜的合金化元素[63]。Shi等[64]制备了Zn-0.8Mn、Zn-0.8Mn-0.4Ag、Zn-0.8Mn-0.4Cu和Zn-0.8Mn-0.4Ca 4种合金,并在同一条件下进行细胞毒性试验。合金元素对细胞存活率的积极影响是Cu > Ca > Ag,在浸提液浓度为80%和60%时表现得最为显著。Li等[65]制备了纯Zn和Zn-4Ag的金属片,同样对其浸提液稀释3倍和L929细胞共培养2 d,纯Zn组细胞活力约106%,而Zn-4Ag组细胞活力约70%。这说明Ag对L929细胞的增殖有很强的负向作用。(3) 合金组织的影响。合金组织对体外细胞毒性最大的影响在于调控锌合金材料的降解性能,影响浸提液中Zn2+的含量。对于不可降解的合金,可以通过体外细胞直接接触法评估组织的影响。对于锌合金,因在细胞培养的过程中释放Zn2+则无法进行评估,只能通过原位植入的方式观察细胞的黏附、生长和迁移。
在研究阶段,锌合金材料表现出体外细胞毒性是否预示临床应用的安全性问题呢?不一定。人体血液中的Zn2+浓度约为120 μmol/L,心脏中高达400 μmol/L[66],远高于体外研究的细胞毒性浓度阈值。在体外细胞毒性试验中,锌合金接触的是开放的极性环境(细胞培养基),与长期植入体内的降解机制和降解产物有显著差异。另外,体外培养的单层细胞,失去了神经体液的调节和细胞间的相互影响,缺乏在体细胞动态平衡的相对稳定环境,对毒性极其敏感。表5分析了可降解医用金属器械/材料与传统不可降解医用金属器械/材料在细胞毒性试验方面的考虑。有研究[67]指出,当前ISO标准(例如ISO 10993-5或ISO 10993-12)不适用于可降解生物金属,需进行适当调整。例如对镁合金的细胞毒性评价,Wang等[68]系统地比较了体内外镁合金的降解速率、产物、pH值、渗透压的影响,按照ISO标准制备材料浸提液,再稀释10倍后与细胞共培养,以便对可降解镁合金进行较可靠的体外细胞毒性评估。通过体内外目标离子浓度的换算求得试验时“最接近临床应用状况”,可能同样适用于可降解锌合金。不同细胞的培养基成分不同,血清蛋白的种类和含量不同,会影响锌合金的降解和细胞对有毒物质的反应,因此建议进一步研究时采用统一的阳性对照做为标准参考,对锌合金临床应用会更具参考意义。
表5 可降解与传统金属植入器械/材料在细胞毒性试验中的异同
Table 5
| Item | Traditional metal implant devices/materials | Degradable metal implant devices/materials |
|---|---|---|
| Material type | Stainless steel, nickel-titanium alloy, cobalt-chromium alloy, titanium alloy, etc. | Zn alloy, Mg alloy, Fe alloy, etc. |
| Property | Inert | Bioactive |
Principle | Support, occupy space, etc., by physical properties to achieve clinical therapeutic effects | Physical properties function in the early stage, then the materials degrade and the target lesion tissue remodels gradually |
Potential source of cytotoxicity | Processing aids, leachables | Processing aids, leachables, degradation products (ions), pH, osmotic pressure, surface energy, etc. |
| Sterilization method | Not limited to ethylene oxide (EO), irradiation sterilization, etc. | Methods with minimal impact on material properties |
| Evaluation endpoint | Morphological evaluation, cell growth ability, and metabolic characteristics (microscopic observation + MTT method, etc.) | |
Contact way | Extraction method, direct or indirect contact method can be selected according to the principle of "closest to the application situation". Generally, the extraction method is recommended | Extraction method, direct or indirect contact method can be selected according to the principle of "closest to the application situation" |
Extraction medium | The ability to support cell growth and to extract both polar and non-polar substances | Cell culture medium with serum, generally. The ratio of serum can be adjusted according to the effect of serum on the material |
Extraction condition | Generally (37 ± 1)oC, (24 ± 2) h | The appropriate extraction time can be selected according to the implantation time, degradation rate and degradation products in vivo. Evaluation of multiple extraction times are also necessary to fully understand and assess biological risks |
| Extraction ratio | (Surface area or mass / volume) ± 10% | |
| Extraction | Dilution is not recommended generally | Multiple dilutions may be necessary |
| Extraction treatment | Adjustment is not recommended generally | Filtration, centrifugation, pH adjustment, etc., can be used, but treatment should be recorded and evaluated |
Cell line | Suitable cell lines recognized by ISO experts, such as mouse fibroblast CCL1 (L929), mouse embryonic fibroblast CCL163 (Balb/3T3 clone A31), etc. L929 cells are generally used in China | Depending on the application site, sensitivity- or site-specific cells may be required to evaluate their cellular responses more objectively |
3.2 锌合金的血液相容性研究
在一项以316L不锈钢、纯Zn和锌合金为对照的研究[83]中,系统评估了Zn-0.8Cu、Zn-0.8Mn和Zn-0.8Li 3种锌合金的血液相容性。研究显示,316L不锈钢、纯Zn、Zn-0.8Cu、Zn-0.8Mn和Zn-0.8Li的溶血率分别为0.38% ± 0.08%、1.04% ± 0.21%、0.47% ± 0.21%、0.57% ± 0.14%和0.52% ± 0.22%。在血小板黏附试验中,锌合金表面的血小板呈圆形,几乎没有伪足扩散。数量上,锌合金与316L不锈钢相比无统计学差异,但明显少于纯Zn组。并且,表面均未观察到明显的血小板活化、血细胞聚集、凝血或补体活化现象。此外,锌合金延长了血液的凝血酶原时间(PT)和部分凝血活酶时间(PTT),暗示了其潜在的抗凝功能。此外,其他研究[72~74]报道的锌合金材料的溶血性能均小于5%,符合ISO标准的要求。因此,锌合金材料的血液相容性良好,满足作为骨科和心血管植入材料的要求。值得一提的是,材料的加工工艺、表面特性等关系着医疗器械终产品的血液相容性的好坏。如锌合金材料制成了与循环血液直接接触的支架等,应基于终产品进行血液相容性的全面评价。
3.3 锌合金的体内试验
为探索锌合金在血管支架方面的应用,Yang等[78]将纯Zn支架植入到兔子主动脉1 a时间,植入期间,兔子动脉内没有出现炎症、血小板聚集、血栓形成和明显的内膜增生,支架降解的过程中血管发生了良性重塑。此外,还发现了与血管重塑过程相匹配的Zn支架降解行为:前6个月内,纯Zn支架可以保持力学完整性,12个月后约40%的支架已经降解。纯Zn在体内的表现证明其做为可降解医用材料的优势,降解速率适宜,生物相容性良好。但是纯Zn的力学性能较差,需要加入合金化元素才能满足特定的应用需求。
Li、Mg、Al的加入(Zn-0.1Li、Zn-0.2Mg、Zn-0.5Mg、Zn-8Mg、Zn-1Al、Zn-3Al、Zn-5Al)改善了力学性能,却使得上述合金在体内(大鼠腹主动脉)的生物学表现更差[79~81]。植入11个月后,在Zn-Li合金组中仍观察到中等程度的慢性炎症反应,并伴非阻塞性的新生内膜增厚[79]。与纯Zn相比,Zn-xMg合金随着Mg含量的增加,生物相容性呈轻微恶化的趋势,炎症细胞浸润和新生内膜活化略有升高。植入6个月时,Zn-8Mg没有显示出明显的内膜增厚,但表现出中等程度的慢性炎症,以及管腔横截面积的减少。植入11个月时,炎症有一定程度消退,但出现内膜增厚,并伴有不连续的内皮细胞[80]。Zn-xAl表现略好,在植入3个月时,仍可观察到中性粒细胞和嗜酸性粒细胞浸润的急性局部炎症。植入6个月时,观察到植入物周围致密的纤维化沉积物,未检测到坏死组织,与周围动脉组织具有可接受的相容性[81]。
在惰性气体保护下,以99.999%高纯Zn和99.995%高纯Cu为原料,经熔炼、轧制、挤出、拉拔、退火、激光雕刻、抛光、酸洗、环氧乙烷灭菌、解析等工艺流程制备的Zn-0.8Cu冠状动脉支架是目前唯一的一款已经中国国家药品监督管理局批准进入人体临床试验的锌合金血管支架。与兔、大鼠等小动物相比,猪的冠状动脉与人体冠状动脉在血管尺寸、解剖学特征、新生内膜生长方面最为相近,因此猪冠状动脉植入模型是评价支架的降解周期、力学性能、降解产物同组织的相容性及组织反应的重要手段[83]。Zn-0.8Cu支架植入猪的冠状动脉长达24个月,结果显示,支架植入后1个月内完成血管内皮化,在植入的24个月内提供了足够的结构支撑并显示出适当的降解速率。支架植入3个月后,支架杆周围聚集有细胞核深染的上皮细胞样巨噬细胞,植入9个月后巨噬细胞浸润减少,并转变为轻度炎症,支架杆降解部分被平滑肌细胞取代。降解产物在支架杆周围形成后,可以分解成小尺寸的产物(< 20 μm)并向血管外膜的方向扩散,而不是滞留在原位成为不易扩散和降解的大尺寸团聚物。腐蚀产物的向外迁移一般有2种可能性,一是通过细胞间途径中的体液,二是通过细胞路径中的细胞吞噬。研究观测到多核异物巨细胞吞噬Zn-0.8Cu支架降解产物碎片的直接证据。在支架植入后6、12和24个月时,检测Zn元素在植入段血管近端5 mm处血管、远端5 mm处血管和心尖部位组织的含量,结果显示,不论是Zn-0.8Cu支架组和不锈钢支架对照组之间,还是植入段血管的远端与近端之间,Zn元素的含量均无显著差异。光学相干断层成像(optical coherence tomography,OCT)观察到新生内膜光滑,没有发现血栓形成或严重的炎症反应[84]。Oliver等[85]观测到Cu在Zn-Ag基合金植入SD大鼠腹主动脉后炎症抑制(inflammation-resistance)的现象,通过细胞免疫荧光染色(immunofluorescence)等方法证实合金中的铜离子促进了植入物表面NO的产生,而NO能够抑制血小板黏附、平滑肌细胞增殖和白细胞黏附等。表6[75,76,78~81,84~86]总结了锌合金在血管中应用的动物试验。
表6 锌合金在血管中应用的动物试验总结[75,76,78~81,84~86]
Table 6
Material | Shape | Disinfection/sterilization | Animal | Implant site | Implant period month | Performance | Ref. |
|---|---|---|---|---|---|---|---|
99.99% pure Zn | Wire, Φ0.25 mm × 15 mm | UV irradiation | SD rats | Abdominal aorta | 1.5, 3, 4.5, 6; 2.5, 4, 6.5 | At 2.5 months of implantation, neoendothelialization was completed. The neointima contains a thin layer of SMCs and an area of low-density inflammatory cells adjacent to the zinc metal layer and within the corrosion layer, with no signs of necrosis. Despite rapid corrosion after 4 months implantation, the thickness of the neointimal layer did not increase over time. Migration and matrix formation of nucleated cells in the corroded area were observed. No inflammatory response, local necrosis, and progressive intimal hyperplasia were observed | |
99.99% pure Zn | Long wire, Φ0.25 mm | 70% ethanol disinfection | SD rats | Abdominal aorta | 1~12, 14, 20 | At 5, 6, and 8 months of implantation, there was higher cell density and chronic inflammation possibly related to stable corrosive activity. Chronic inflammation subsided between 10 and 20 months. No clear evidence of large-scale cytotoxicity was detected at any time point | [86] |
99.995% pure Zn | Stents, Φ3.0 mm × 10 mm, strut thickness: 165 μm | - | Japanese rabbits | Abdominal aorta | 1, 3, 6, 12 | No significant platelet adhesion or membranous thrombosis was observed after 3 d implantation. Neointimal coverage was observed at 1 month, indicating rapid endothelialization. No significant intimal hyperplasia or lumen loss was found at any time point, and no severe inflammation, platelet aggregation, or thrombosis was observed | [78] |
Zn-0.1Li | Wire, Φ0.25 mm × 10 mm | - | SD rats | Abdominal aorta | 2, 4, 6.5, 9, 12 | At 11 months postimplantation, moderate chronic inflammation with non-obstructive neointima was still observed in the Zn-Li alloy group. Biocompatibility is slightly worse than pure Zn | [79] |
| Material | Shape | Disinfection/ | Animal | Implant site | Implant | Performance | Ref. |
| sterilization | period | ||||||
| month | |||||||
Zn, Zn-xMg (x = 0.2, 0.5, 8) | Wire, 15 mm segment | Disinfection | SD rats | Abdominal aorta | 1.5, 3, 4.5, 6, 11 | Compared with pure Zn, the biocompatibility of Zn-xMg alloy showed a slight deterioration trend with the increase of Mg content. The inflammatory cell infiltration and neointima activation increased slightly. At 6 months, Zn-8Mg did not show significant intimal thickening, but exhibited moderate chronic inflammation and a reduction in the cross-sectional area of the lumen. At 11 months, inflammation had some resolution, but intimal thickening with discontinuous endothelial cells was appeared. It is speculated that Mg2Zn11 particles may induce deleterious macrophage responses thus disrupting the positive remodeling effect of Zn | [80] |
Zn-xAl (x = 1, 3, 5) | Strip, 12 mm × 300 μm × 300 μm | 70% ethanol disinfection | SD rats | Abdominal aorta | 1.5, 3, 4.5, 6 | At 3 months of implantation, acute local inflammation with neutrophilic and eosinophilic infiltration was still observed. At 6 months, dense fibrotic deposits around the implant were observed, no necrotic tissue was detected. Zn-xAl had acceptable compatibility with surrounding arterial tissue | [81] |
Zn-0.8Cu | Stent, Φ3.0 mm × 20 mm, wall thickness: ~127 μm | EO sterilization | White pigs | Coronary artery | 1, 3, 6, 9, 12, 18, 24 | Vascular endothelialization was completed within 1 months after stent implantation. ZnCu stent provided adequate structural support and exhibited an appropriate rate of degradation within 24 months, with no accumulation of degradation products, thrombosis or inflammatory responses | [84] |
Zn-4Ag, Zn-4Ag-0.6Mn, Zn-4Ag- 0.8Cu-0.6Mn-0.15Zr | Wire, Φ0.25 mm × 15 mm | Disinfection | SD rats | Abdominal aorta | 3, 6 | At 6 months of implantation, a significant reduction of inflammatory activities was found in the quinary alloy relative to the other Zn-based materials. And inflammation, but not smooth muscle cell hyperplasia, is correlated with neointimal growth for the Zn-Ag-based alloys | [85] |
尽管Zn-0.1Li在大鼠腹主动脉观察到长达11个月的慢性炎症反应和内膜增生,但是Zn-0.4Li金属片在大鼠股骨的表现非常好,纯Zn和Zn-0.4Li植入部位均未见骨溶解、变形、脱位或气影,与术后即刻相比,术后8周相邻皮质骨显示出更高的放射学密度,表明周围成骨。与纯Zn相比,Zn-0.4Li植入物周围观察到更多的胶原蛋白和新骨组织[87]。精加工成多孔支架的Zn-0.8Mn、Zn-0.8Sr合金也表现出令人满意的结果。Zn-0.8Mn支架植入大鼠股骨外侧髁处缺损,术后4周可见新骨形成,术后8和12周支架周围出现大量新骨组织,骨小梁也比纯Ti组更厚,在体内显示出良好的成骨性能和生物相容性,在器官中也没有锌离子积累[88]。Zn-0.8Sr支架同样表现出良好的骨缺损修复性能和骨生长趋势,无炎症反应[89]。Zn-0.5Mn植入大鼠胫骨4个月后,观察到健康的骨和血管,骨髓病理切片显示骨髓增生,不影响肝肾功能[90]。除此之外,Zn-0.4Fe、Zn-0.4Cu、Zn-2.0Ag、Zn-0.8Mg、Zn-0.8Ca、Zn-0.1Sr和Zn-0.1Mn在植入大鼠股骨后,也表现出良好的生物相容性,无骨溶解、畸形或脱位的迹象[91]。随着时间的推移,植入物周围的皮质骨变厚,放射学密度变高,表明周向成骨。以上结果支持了不同合金元素的锌合金在骨科的应用前景。
表7 锌合金在骨科及其他组织应用的动物试验总结[87~93]
Table 7
| Material | Shape | Disinfection/Sterilization | Animal | Implant site | Implant period | Performance | Ref. |
|---|---|---|---|---|---|---|---|
Zn, Zn-0.4Li | Rod, Φ1.6 mm × 15 mm | - | SD rats | Femoral | 2 months | Neither pure Zn nor Zn-0.4Li implanted sites showed osteolysis, deformation, dislocation, or air shadows. Compared to immediate postoperation, the adjacent cortical bone showed higher radiographic densities at 8 weeks postoperation, indicating peripheral osteogenesis. Compared with pure Zn, more collagen and new bone tissue were observed around the Zn-0.4Li implants | [87] |
Zn-0.8Mn, Zn-0.8Sr | Porous scaffold | - | Rats | Femoral condyle | 4, 8, and 12 weeks | New bone formation was observed at 4 weeks after Zn-0.8Mn implantation, and a large amount of new bone tissue was observed around the scaffold at 8 and 12 weeks postoperation. The trabecular bone was thicker than that of pure Ti group. Zn-0.8Mn scaffold showed good osteogenic performance and biocompatibility in vivo. Zn ions were not accumulated in the organs. Zn-0.8Sr scaffold also has good bone defect repair performance and growth tendency without inflammatory reaction | [88, 89] |
Zn-0.5Mn | Φ1.5 mm × 5 mm | UV disinfection | SD rats | Tibia | 4 months | After 4 months implantation, healthy bone and blood vessels were observed, bone marrow hyperplasia was showed by pathological sections, liver and kidney functions were not affected | [90] |
Zn-0.4Fe, Zn-0.4Cu, Zn-2.0Ag, Zn-0.8Mg, Zn-0.8Ca, Zn-0.1Sr, Zn-0.4Li, Zn-0.1Mn | Rod, Φ1.6 mm × 15 mm | - | SD rats | Femoral | 2 months | The cortical bone surrounding the implant thickened and radiographic dense increased, indicating circumferential osteogenesis. All implants were biocompatible with no evidence of osteolysis, deformity or dislocation. At 2 months implantation, new bone was formed and contacted the implants directly | [91] |
Zn, Zn-2Fe | Φ7 mm × 2 mm | - | Wistar rats | Subcutaneous tissue of back | 4, 8, 12, 18, 24 weeks | No tissue inflammation or necrosis was observed | [93] |
Zn-0.8Li-0.1Mn | Gastroin-testinal staple | Disinfection | Mini fragrant pigs | Gastrointestinal anastomosis | 3 d, 8 weeks, 12 weeks | In the early stage after surgery, there were a small amount of inflammatory cells (mainly neutrophils and lymphocytes) and macrophages around the Zn-Li-Mn and Ti alloy nails. Inflammation cells around the Zn-Li-Mn alloy nails were slightly less than the Ti alloy group. At 12 weeks postoperation, new gastrointestinal tissues were found around the nails in both groups, the tissues healed well, and the number of inflammatory cells was significantly reduced | [92] |
4 总结与展望
适宜的腐蚀速率、良好的力学性能和生物活性,使锌合金成为被寄予厚望的可降解生物医用金属材料。近年来,研究者们对锌合金的成分设计、加工制备过程、内部组织结构、表面改性及降解机理等方面进行了大量系统研究,不断优化其力学性能、腐蚀速率及生物相容性,并积极拓展其临床应用范围。本文根据材料与机体相互作用的方式,总结了对锌合金器械进行生物相容性评价的原则和方法。但是材料植入后的机体反应及机体与材料(器械)的相互作用极其复杂,是一个联系的、动态的、长期的生理过程,从基础研究到产品定型和优化需要经历漫长的过程,对新型可降解植入器械的临床试验或者应用应该持乐观且谨慎的态度。展望未来,仍有几点生物相容性方面的考虑需要被重视。
(1) 尽管多数研究支持锌合金在动物体内的生物相容性,但其降解过程中腐蚀产物层中金属间颗粒的富集、吸收和转运及其对组织再生的影响仍然令人担忧。如何对锌合金降解产物进行荧光标记,追踪降解产物的吸收、转运过程及相应的生物学表现,将是一项重大课题。
(2) 终产品植入物在运动疲劳中产生的应力损伤是否引起局部腐蚀甚至点蚀,从而导致植入物提前失效引起机体更多的物理损伤也是生物相容性研究的一个方面。另外,锌合金植入物与其他金属植入物配合使用可能会产生电偶腐蚀,改变产品临床预期的降解速率,这种情况下的使用顺序、空间和时间距离的安全性也应该有所考虑。
(3) 体外的细胞毒性评价作为一套敏感的毒性筛选系统,其作用仍然不可小觑。如何考虑局部微环境中细胞类型、蛋白、溶解O2的影响,结合体内降解速率、降解产物积累和周围细胞的表现,建立适当的细胞毒性评价体系对于可降解锌合金的临床应用具有重要意义,也可以做为一项锌合金加工设计时的体外筛选系统。
(4) 锌合金降解过程中导致局部Zn2+浓度增加,Zn2+参与体内多种生理活动,应在时间效应和剂量效应下研究过量Zn2+触发的信号通路、蛋白合成、物质转运对机体的影响,是否会存在生理调控之外的信号通路激活,降解产物对周围细胞包括炎症细胞在分子水平的影响等。近年来分子生物学和生物信息学发展出的基因组学、蛋白质组学和代谢组学研究也可联合应用于识别降解产物潜在的基因和细胞毒性。
参考文献
Materials for microfabricated implantable devices: A review
[J].The application of microfabrication to the development of biomedical implants has produced a new generation of miniaturized technology for assisting treatment and research. Microfabricated implantable devices (μID) are an increasingly important tool, and the development of new μIDs is a rapidly growing field that requires new microtechnologies able to safely and accurately function in vivo. Here, we present a review of μID research that examines the critical role of material choice in design and fabrication. Materials commonly used for μID production are identified and presented along with their relevant physical properties and a survey of the state-of-the-art in μID development. The consequence of material choice as it pertains to microfabrication and biocompatibility is discussed in detail with a particular focus on the divide between hard, rigid materials and soft, pliable polymers.
Bio-functionalization of biomedical metals
[J].
Magnesium-based biodegradable alloys: Degradation, application, and alloying elements
[J].
Bioresorbable coronary scaffold technologies: What's new?
[J].To overcome the not negligible metallic drug-eluting stents adverse events rate, the polymeric or metallic bioresorbable scaffolds were designed to provide early drug delivery and mechanical support followed by complete resorption. However, the long-term evidence, focusing on the leading Absorb BVS technology, showed higher events compared with drug-eluting stents. This review discusses the lights and shadows of the current bioresorbable scaffolds according to their mechanical properties and biodegradation profile and suggests possible perspective on these technologies. Improved scaffold design and deployment techniques might mitigate early bioresorbable scaffolds risk enhancing the late benefit of complete resorption.Copyright © 2020 Elsevier Inc. All rights reserved.
Fully bioresorbable vascular scaffolds: Lessons learned and future directions
[J].Fully bioresorbable scaffolds (BRS) were designed to overcome the limitations of metallic drug-eluting stents, which permanently cage the vessel wall, thereby preventing normal coronary vasomotion, preclude bypass grafting and can provoke long-term foreign-body responses. Although multiple scaffolds have been or are in development, the Absorb Bioresorbable Vascular Scaffold (BVS; Abbott Vascular) was the first FDA-approved device and was widely expected to fulfil the dream of interventional cardiologists of a transient scaffold that would disappear 'when the job was done' and would not hamper further treatment options. Although early, small studies and even large, randomized trials showed beneficial outcomes up to 1 year of follow-up, longer-term results have been disappointing, with increased rates of device thrombosis and target-lesion revascularization. The Absorb BVS device was withdrawn from the market because of low demand. In this Review, we summarize the preclinical and clinical data available for BRS to understand how the vascular biological reactions to these devices differ from biological reactions to metallic drug-eluting stents and how these responses translate into clinical outcomes. We also discuss next-generation BRS and outline modifications that are needed to improve the long-term outcomes with these devices so that they eventually become a viable option for patients with symptomatic obstructive coronary artery disease.
Freeing the vessel from metallic cage: What can we achieve with bioresorbable vascular scaffolds?
[J].
Bioresorbable vascular scaffolds: Time to absorb past lessons or fade away?
Advances in biodegradable vascular stent materials
[J].
Mechanical strength, biodegradation, and in vitro and in vivo biocompatibility of Zn biomaterials
[J].
Biodegradable iron-based materials-what was done and what more can Be done?
[J].
The microstructure, mechanical properties and degradation behavior of laser-melted Mg-Sn alloys
[J].
Laser additive manufacturing of Zn metal parts for biodegradable applications: Processing, formation quality and mechanical properties
[J].
Vacuum heat treatment of iron parts produced by selective laser melting: Microstructure, residual stress and tensile behavior
[J].
Excellent age hardenability with the controllable microstructure of AXW100 magnesium sheet alloy
[J].Age-hardenability and corresponding improvement of the mechanical properties of Mg-1Al-0.7Ca and Mg-1Al-0.7Ca-0.7Y alloy sheets are addressed with respect to the microstructure and texture evolution during thermomechanical treatments. A fine grain structure and weak texture with the basal pole split into the sheet transverse direction are retained in the Mg-1Al-0.7Ca-0.7Y sheet even after the homogenization at 500 °C, due to the grain boundary pinning by Y-containing precipitates possessing a high thermal stability. Contrarily, the Mg-1Al-0.7Ca sheet shows a coarse microstructure and basal-type texture after the homogenization. The peak-aged condition is attained after the aging at 250 °C for 1800 s of both homogenized sheets, while the Y-containing sheet shows a higher hardness than the Mg-1Al-0.7Ca sheet. TEM analysis and thermodynamic calculation show the formation of metastable precipitates composed of Al, Ca, Y and Mg in the Mg-1Al-0.7Ca-0.7Y sheet at the homogenized and peak-aged conditions. A significant increase in the yield strength is obtained in the peak-aged condition from 162 MPa after the homogenization to 244 MPa, which arises from the increased size and number density of the precipitates. The high age-hardenability of the Mg-1Al-0.7Ca-0.7Y sheet attributes to the superior mechanical properties with an improved ductility promoted by the weak texture.
The important rule of material and chemical characterization in device evaluation
[J].
医疗器械生物材料表征和化学性能检测的重要性
[J].
The role of rare earth elements in biodegradable metals: A review
[J].
Fundamental theory of biodegradable metals—Definition, criteria, and design
[J].
Processing of a novel Zn alloy micro-tube for biodegradable vascular stent application
[J].In recent years, zinc based alloys as a new biodegradable metal material aroused intensive interests. However, the processing of Zn alloys micro-tubes (named slender-diameter and thin-walled tubes) is very difficult due to their HCP crystal structure and unfavorable mechanical properties. This study aimed to develop a novel technique to produce micro-tube of Zn alloy with good performance for biodegradable vascular stent application. In the present work, a processing method that combined drilling, cold rolling and optimized drawing was proposed to produce the novel Zn-5Mg-1Fe (wt%) alloy micro-tubes. The micro-tube with outer diameter of 2.5?mm and thickness of 130?μm was fabricated by this method and its dimension errors are within 10?μm. The micro-tube exhibits a fine and homogeneous microstructure, and the ultimate tensile strength and ductility are more than 220?MPa and 20% respectively. In addition, the micro-tube and stents of Zn alloy exhibit superior in vitro corrosion and expansion performance. It could be concluded that the novel Zn alloy micro-tube fabricated by above method might be a promising candidate material for biodegradable stent.
Additively manufactured biodegrabable metal implants
[J].Additive manufacturing (AM) can produce complicated structures accurately and freely, giving the implant a macro and micro geometry, which makes the implant match the patient's defect site and realize the needs for personalized clinical treatment. Thus, AM provides a new manufacturing method for biodegradable metals. Presently, biodegradable metals are the hotspot issues of metallic biomaterials research. Additively-manufactured biodegradable metals are new research field. In this paper, a comprehensive review on the AM of Mg-, Zn-, and Fe-based biodegradable metals, which focuses on their processes and influencing factors, mechanical properties, biodegradation behavior, and biocompatibility, is given. Finally, the future development trend of the AM biomedical metallic materials is explored.
增材制造可降解金属医用植入物
[J].增材制造技术由于其高精度、高自由度等特点,可赋予医用金属植入物定制化的宏观与微观结构,使植入物与患者待修复缺损部位实现更好的生物力学适配,满足临床治疗个性化方案的需求,并为医用金属植入物的制造提供新途径。可降解金属目前是医用金属的研究热点,增材制造可降解金属医用植入物是个新方向,本文重点对增材制造镁基、锌基、铁基可降解金属的工艺流程及影响因素、力学性能、降解行为、生物相容性相关结果进行分析与总结,并展望了增材制造技术在医用可降解金属植入物领域的未来发展方向。
Current status and perspectives of zinc-based absorbable alloys for biomedical applications
[J].Absorbable metals have the potential to serve as the next generation of temporary medical implant devices by safely dissolving in the human body upon vascular tissue healing and bone regeneration. Their implementation in the market could greatly reduce the need of costly and risky additional surgeries for either implant replacement or removal, often required in current permanent implants. Despite the extensive research done over the last two decades on magnesium (Mg) and iron (Fe) based alloys, they have not generally shown a satisfactory combination of mechanical properties, biocompatibility and controlled degradation rate in the physiological environment. Consequently, zinc (Zn) based alloys were introduced in the last few years as alternative materials to overcome the limitations of Fe and Mg-based alloys. The blend of different alloying elements and processing conditions have led to a wide variety of Zn-based alloys having tunable mechanical properties and corrosion rates. This review provides the most recent progress in the development of absorbable Zn-based alloys for biomedical implant applications, primarily for cardiovascular and orthopedic devices. Their biocompatibility, processability and metallurgical aspects, as well as their mechanical behavior and corrosion properties are presented and discussed, including their opportunities, limitations and future research directions. STATEMENT OF SIGNIFICANCE: Temporary orthopedic bioimplants have become increasingly popular as they offer an alternative to prevent complications, like infections or secondary surgeries, often related to the implantation of permanent devices. Iron and magnesium alloys were extensively studied as candidates for absorbable medical applications, but they generally failed to provide a desirable mechanical performance and corrosion characteristics in the physiological environment. Zinc was introduced in the last decade as a potential implant material after showing outstanding biocompatibility and biodegradability. This review summarizes the research advances to date and provides a thorough discussion of the future challenges of absorbable zinc alloys to satisfy the demanding clinical benchmarks for absorbable medical applications. Their biocompatibility, mechanical, and corrosion aspects, both in vitro and in vivo, are comprehensively reviewed and assessed accordingly.Copyright © 2019 Acta Materialia Inc. Published by Elsevier Ltd. All rights reserved.
Degradation of zinc in saline solutions, plasma, and whole blood
[J].
Zinc-based biomaterials for regeneration and therapy
[J].Zinc has been described as the 'calcium of the twenty-first century'. Zinc-based degradable biomaterials have recently emerged thanks to their intrinsic physiological relevance, biocompatibility, biodegradability, and pro-regeneration properties. Zinc-based biomaterials mainly include: metallic zinc alloys, zinc ceramic nanomaterials, and zinc metal-organic frameworks (MOFs). Metallic zinc implants degrade at a desirable rate, matching the healing pace of local tissues, and stimulating remodeling and formation of new tissues. Zinc ceramic nanomaterials are also beneficial for tissue engineering and therapy thanks to their nanostructures and antibacterial properties. MOFs have large surface areas and are easily functionalized, making them ideal for drug delivery and cancer therapy. This review highlights recent developments in zinc-based biomaterials, discusses obstacles to overcome, and pinpoints directions for future research.Copyright © 2018 Elsevier Ltd. All rights reserved.
Roles of zinc signaling in the immune system
[J].
The galvanization of biology: A growing appreciation for the roles of zinc
[J].Zinc ions are key structural components of a large number of proteins. The binding of zinc stabilizes the folded conformations of domains so that they may facilitate interactions between the proteins and other macromolecules such as DNA. The modular nature of some of these zinc-containing proteins has allowed the rational design of site-specific DNA binding proteins. The ability of zinc to be bound specifically within a range of tetrahedral sites appears to be responsible for the evolution of the side range of zinc-stabilized structural domains now known to exist. The lack of redox activity for the zinc ion and its binding and exchange kinetics also may be important in the use of zinc for specific functional roles.
Role of nutritional zinc in the prevention of osteoporosis
[J].Zinc is known as an essential nutritional factor in the growth of the human and animals. Bone growth retardation is a common finding in various conditions associated with dietary zinc deficiency. Bone zinc content has been shown to decrease in aging, skeletal unloading, and postmenopausal conditions, suggesting its role in bone disorder. Zinc has been demonstrated to have a stimulatory effect on osteoblastic bone formation and mineralization; the metal directly activates aminoacyl-tRNA synthetase, a rate-limiting enzyme at translational process of protein synthesis, in the cells, and it stimulates cellular protein synthesis. Zinc has been shown to stimulate gene expression of the transcription factors runt-related transcription factor 2 (Runx2) that is related to differentiation into osteoblastic cells. Moreover, zinc has been shown to inhibit osteoclastic bone resorption due to inhibiting osteoclast-like cell formation from bone marrow cells and stimulating apoptotic cell death of mature osteoclasts. Zinc has a suppressive effect on the receptor activator of nuclear factor (NF)-kappaB ligand (RANKL)-induced osteoclastogenesis. Zinc transporter has been shown to express in osteoblastic and osteoclastic cells. Zinc protein is involved in transcription. The intake of dietary zinc causes an increase in bone mass. beta-Alanyl-L: -histidinato zinc (AHZ) is a zinc compound, in which zinc is chelated to beta-alanyl-L: -histidine. The stimulatory effect of AHZ on bone formation is more intensive than that of zinc sulfate. Zinc acexamate has also been shown to have a potent-anabolic effect on bone. The oral administration of AHZ or zinc acexamate has the restorative effect on bone loss under various pathophysiologic conditions including aging, skeletal unloading, aluminum bone toxicity, calcium- and vitamin D-deficiency, adjuvant arthritis, estrogen deficiency, diabetes, and fracture healing. Zinc compounds may be designed as new supplementation factor in the prevention and therapy of osteoporosis.
KRAB zinc-finger proteins contribute to the evolution of gene regulatory networks
[J].
Nutritional implications in vascular endothelial cell metabolism
[J].Endothelial cells interact with blood components and the abluminal tissues, thus playing an active role in many aspects of vascular function. Numerous physiologic and pathophysiologic stimuli are often mediated by nutrients that can contribute to the overall functions of endothelial cells in the regulation of vascular tone, coagulation, cellular growth, immune and inflammatory responses. Therefore, nutrient-mediated functional changes of the endothelium and the underlying tissues may be significantly involved in disease processes such as atherosclerosis. There is evidence that individual nutrients or nutrient derivatives may either provoke or prevent metabolic and physiologic perturbations of the vascular endothelium. Diets high in fat and/or calories are considered a risk factor for the development of atherosclerosis. Our research has shown that certain diet-derived lipids and their derivatives can disrupt normal endothelial integrity, thus reducing the ability of the endothelium to act as a selectively permeable barrier to blood components. Mechanisms underlying fatty acid-mediated endothelial cell dysfunction may be related to changes in fatty acid composition as well as to an increase in cellular oxidative stress. Selective lipid accumulation and fatty acid changes in endothelial cells can modulate membrane fluidity, proteoglycan metabolism and signal transduction mechanisms. Most importantly, dietary fats rich in certain unsaturated fatty acids, may be atherogenic by enhancing the formation of reactive oxygen intermediates. A subsequent imbalance in cellular oxidative stress/antioxidant status can activate oxidative stress-responsive transcription factors, which in turn may promote cytokine production, expression of adhesion molecules on the surface of endothelial cells, and thus intensify an inflammatory response in atherosclerosis. Our data also suggest that certain nutrients, which have antioxidant and/or membrane stabilizing properties, can protect endothelial cells by interfering with lipid/cytokine-mediated endothelial cell dysfunction. These findings contribute to the understanding of the interactive role of dietary fats with inflammatory components, as well as with nutrients that exhibit antiatherogenic properties, in the development of atherosclerosis.
Nutritional factors and bone homeostasis: Synergistic effect with zinc and genistein in osteogenesis
[J].Bone homeostasis is regulated through osteoclasts and osteoblasts. Osteoporosis, which is induced with its accompanying decrease in bone mass with increasing age, is widely recognized as a major public health problem. Bone loss may be due to decreased osteoblastic bone formation and increased osteoclastic bone resorption. There is growing evidence that nutritional and food factors may play a part in the prevention of bone loss with aging and have been to be worthy of notice in the prevention of osteoporosis. Zinc, an essential trace element, or genistein, which are contained in soybeans, has been shown to have a stimulatory effect on osteoblastic bone formation and an inhibitory effect on osteoclastic bone resorption, thereby increasing bone mass. These factors have an effect on protein synthesis and gene expression, which are related to bone formation in osteoblastic cells and bone resorption in osteoclastic cells. The combination of zinc and genistein is found to reveal the synergistic effect on bone anabolic effect. The oral administration of those factors has been shown to prevent on bone loss in ovariectomized rats, an animal model for osteoporosis, indicating a role in the prevention of osteoporosis. Supplemental intake of ingredient with the combination of zinc and genistein has been shown to have a preventive effect on osteoporosis in human subjects, suggesting a role in the prevention of bone loss.
A mathematical model of zinc absorption in humans as a function of dietary zinc and phytate
[J].The quantities of zinc and phytate in the diet are the primary factors determining zinc absorption. A mathematical model of zinc absorption as a function of dietary zinc and phytate can be used to predict dietary zinc requirements and, potentially, enhance our understanding of zinc absorption. Our goal was to develop a model of practical and informative value based on fundamental knowledge of the zinc absorption process and then fit the model to selected published data to assess its validity and estimate parameter values. A model of moderate mathematical complexity relating total zinc absorption to total dietary zinc and total dietary phytate was derived and fit to 21 mean data from whole day absorption studies using nonlinear regression analysis. Model validity, goodness of fit, satisfaction of regression assumptions, and quality of the parameter estimates were evaluated using standard statistical criteria. The fit had an R(2) of 0.82. The residuals were found to exhibit a normal distribution, constant variance, and independence. The parameters of the model, A(MAX), K(R), and K(P), were estimated to have values of 0.13, 0.10, and 1.2 mmol/d, respectively. Several of these estimates had wide CI attributable in part to the small number and the scatter of the data. The model was judged to be valid and of immediate value for studying and predicting absorption. A version of the model incorporating a passive absorption mechanism was not supported by the available data.
Zinc: the brain's dark horse
[J].
Recent research and progress of biodegradable zinc alloys and composites for biomedical applications: Biomechanical and biocorrosion perspectives
[J].Biodegradable metals (BMs) gradually degrade by releasing corrosion products once exposed to the physiological environment in the body. Complete dissolution of biodegradable implants assists tissue healing, with no implant residues in the surrounding tissues. In recent years, three classes of BMs have been extensively investigated, including magnesium (Mg)-based, iron (Fe)-based, and zinc (Zn)-based BMs. Among these three BMs, Mg-based materials have undergone the most clinical trials. However, Mg-based BMs generally exhibit faster degradation rates, which may not match the healing periods for bone tissue, whereas Fe-based BMs exhibit slower and less complete degradation. Zn-based BMs are now considered a new class of BMs due to their intermediate degradation rates, which fall between those of Mg-based BMs and Fe-based BMs, thus requiring extensive research to validate their suitability for biomedical applications. In the present study, recent research and development on Zn-based BMs are reviewed in conjunction with discussion of their advantages and limitations in relation to existing BMs. The underlying roles of alloy composition, microstructure, and processing technique on the mechanical and corrosion properties of Zn-based BMs are also discussed.© 2020 [The Author/The Authors].
Zinc-nutrient element based alloys for absorbable wound closure devices fabrication: Current status, challenges, and future prospects
[J].
Improved mechanical, degradation, and biological performances of Zn-Fe alloys as bioresorbable implants
[J].Zinc (Zn) is a promising bioresorbable implant material with more moderate degradation rate compared to magnesium (Mg) and iron (Fe). However, the low mechanical strength and localized degradation behavior of pure Zn limit its clinical applications. Alloying is one of the most effective ways to overcome these limitations. After screening the alloying element candidates regarding their potentials for improvement on the degradation and biocompatibility, we proposed Fe as the alloying element for Zn, and investigated the and performances of these alloys in both subcutaneous and femoral tissues. Results showed that the uniformly distributed secondary phase in Zn-Fe alloys significantly improved the mechanical property and facilitated uniform degradation, which thus enhanced their biocompatibility, especially the Zn-0.4Fe alloy. Moreover, these Zn-Fe alloys showed outstanding antibacterial property. Taken together, Zn-Fe alloys could be promising candidates as bioresorbable medical implants for various cardiovascular, wound closure, and orthopedic applications.© 2022 The Authors.
Additively manufactured pure zinc porous scaffolds for critical-sized bone defects of rabbit femur
[J].Additive manufacturing has received attention for the fabrication of medical implants that have customized and complicated structures. Biodegradable Zn metals are revolutionary materials for orthopedic implants. In this study, pure Zn porous scaffolds with diamond structures were fabricated using customized laser powder bed fusion (L-PBF) technology. First, the mechanical properties, corrosion behavior, and biocompatibility of the pure Zn porous scaffolds were characterized. The scaffolds were then implanted into the rabbit femur critical-size bone defect model for 24 weeks. The results showed that the pure Zn porous scaffolds had compressive strength and rigidity comparable to those of cancellous bone, as well as relatively suitable degradation rates for bone regeneration. A benign host response was observed using hematoxylin and eosin (HE) staining of the heart, liver, spleen, lungs, and kidneys. Moreover, the pure Zn porous scaffold showed good biocompatibility and osteogenic promotion ability. This study showed that pure Zn porous scaffolds with customized structures fabricated using L-PBF represent a promising biodegradable solution for treating large bone defects.© 2022 The Authors.
Biological responses to materials
[J].
On the mechanisms of biocompatibility
[J].The manner in which a mutually acceptable co-existence of biomaterials and tissues is developed and sustained has been the focus of attention in biomaterials science for many years, and forms the foundation of the subject of biocompatibility. There are many ways in which materials and tissues can be brought into contact such that this co-existence may be compromised, and the search for biomaterials that are able to provide for the best performance in devices has been based upon the understanding of all the interactions within biocompatibility phenomena. Our understanding of the mechanisms of biocompatibility has been restricted whilst the focus of attention has been long-term implantable devices. In this paper, over 50 years of experience with such devices is analysed and it is shown that, in the vast majority of circumstances, the sole requirement for biocompatibility in a medical device intended for long-term contact with the tissues of the human body is that the material shall do no harm to those tissues, achieved through chemical and biological inertness. Rarely has an attempt to introduce biological activity into a biomaterial been clinically successful in these applications. This essay then turns its attention to the use of biomaterials in tissue engineering, sophisticated cell, drug and gene delivery systems and applications in biotechnology, and shows that here the need for specific and direct interactions between biomaterials and tissue components has become necessary, and with this a new paradigm for biocompatibility has emerged. It is believed that once the need for this change is recognised, so our understanding of the mechanisms of biocompatibility will markedly improve.
Biocompatibility evaluation of medical devices: Status, progress and trend
[J].
医疗器械生物相容性评价: 现状、进展与趋势
[J].
On the nature of biomaterials
[J].The situations in which biomaterials are currently used are vastly different to those of just a decade ago. Although implantable medical devices are still immensely important, medical technologies now encompass a range of drug and gene delivery systems, tissue engineering and cell therapies, organ printing and cell patterning, nanotechnology based imaging and diagnostic systems and microelectronic devices. These technologies still encompass metals, ceramics and synthetic polymers, but also biopolymers, self assembled systems, nanoparticles, carbon nanotubes and quantum dots. These changes imply that our original concepts of biomaterials and our expectations of their performance also have to change. This Leading Opinion Paper addresses these issues. It concludes that many substances which hitherto we may not have thought of as biomaterials should now be considered as such so that, alongside the traditional structural biomaterials, we have substances that have been engineered to perform functions within health care where their performance is directly controlled by interactions with tissues and tissue components. These include engineered tissues, cells, organs and even viruses. This essay develops the arguments for a radically different definition of a biomaterial.
Biocompatibility of dental casting alloys
[J].Most cast dental restorations are made from alloys or commercially pure titanium (cpTi). Many orthodontic appliances are also fabricated from metallic materials. It has been documented in vitro and in vivo that metallic dental devices release metal ions, mainly due to corrosion. Those metallic components may be locally and systemically distributed and could play a role in the etiology of oral and systemic pathological conditions. The quality and quantity of the released cations depend upon the type of alloy and various corrosion parameters. No general correlation has been observed between alloy nobility and corrosion. However, it has been documented that some Ni-based alloys, such as beryllium-containing Ni alloys, exhibit increased corrosion, specifically at low pH. Further, microparticles are abraded from metallic restorations due to wear. In sufficient quantities, released metal ions-particularly Cu, Ni, Be, and abraded microparticles-can also induce inflammation of the adjacent periodontal tissues and the oral mucosa. While there is also some in vitro evidence that the immune response can be altered by various metal ions, the role of these ions in oral inflammatory diseases such as gingivitis and periodontitis is unknown. Allergic reactions due to metallic dental restorations have been documented. Ni has especially been identified as being highly allergenic. Interestingly, from 34% to 65.5% of the patients who are allergic to Ni are also allergic to Pd. Further, Pd allergy always occurrs with Ni sensitivity. In contrast, no study has been published which supports the hypothesis that dental metallic materials are mutagenic/genotoxic or might be a carcinogenic hazard to man. Taken together, very contradictory data have been documented regarding the local and systemic effects of dental casting alloys and metallic ions released from them. Therefore, it is of critical importance to elucidate the release of cations from metallic dental restorations in the oral environment and to determine the biological interactions of released metal components with oral and systemic tissues.
Pathogenic mechanisms and therapeutic implication in nickel-induced cell damage
[J].
Evaluation of metal allergies in patients with coronary stents
[J].In-stent restenosis is a complication which impairs the success of coronary stenting. Recently, it was supposed that a delayed hypersensitivity reaction to nickel and molybdenum might be one of the triggering factors in in-stent restenosis. We have analyzed the data collected in our centre with respect to this hypothesis. Altogether, 34 patients were investigated (24 male, 10 female). Patch tests were performed with the standard series of the German Contact Dermatitis Research Group and a metal series containing the metal components of 316 L stainless steel. A positive patch test reaction to nickel was observed in 4 (11.8%) patients. None of the patients showed sensitization to the other metals. Retrospective analysis was performed in 20 patients: 2 of these patients had a positive patch test reaction to nickel, one of whom had an in-stent restenosis, and the other not. Restenoses were predominantly observed in patients with negative patch test reactions to nickel (6/18 patients). Out of the patients who were investigated prospectively only one showed sensitization to nickel. Restenosis was observed in 2 patients: neither patient had nickel allergy. Although it still cannot be excluded that metal allergy may play a role in the restenosis process in coronary stenting, there is at present little evidence for it.
Evaluation of in-stent stenosis by magnetic resonance phase-velocity mapping in nickel-titanium stents
[J].To evaluate different grades of in-stent stenosis in a nickel-titanium stent with MRI.Magnetic resonance phase velocity mapping (MR-PVM) was used to measure flow velocity through a 9-mm NiTi stent with three different degrees of stenosis in a phantom study. The tested stenotic geometries were 1) axisymmetric 75%, 2) axisymmetric 90%, and 3) asymmetric 50%. The MR-PVM data were subsequently compared with the velocities from computational fluid dynamic (CFD) simulations of identical conditions.Good quantitative agreement in velocity distribution for the 50% and 75% stenoses was observed. The agreement was poor for the 90% stenosis, most likely due to turbulence and the high-velocity gradients found in the small luminal area relative to the pixel resolution in our imaging settings.The accuracy of the MRI velocities inside the stented area renders MRI a modality that may be used to assess moderate to severe in-stent restenosis (ISR) in medium-sized vascular stents in peripheral vessels, such as the iliac, carotid, and femoral arteries. Advances in MR instrumentation may provide sufficient resolution to obtain adequate velocity information from smaller vessels, such as the coronary arteries, and allow MRI to substitute for invasive and expensive catheterization procedures currently in clinical use.(c) 2005 Wiley-Liss, Inc.
Development in applications of porous metals
[J].
Research process on property and application of metal porous materials
[J].
The cellular and molecular biology of periprosthetic osteolysis
[J].
Wear particulate and osteolysis
[J].
Bacterial anti-adhesion surface design: Surface patterning, roughness and wettability: A review
[J].Bacterial adhesion and biofilm formation impose a heavy burden on the medical system. Bacterial adhesion on implant materials would induce inflammation and result in implant failure. The adhesion of bacteria on food-processing and handling equipment may lead to food-borne illness. To reduce and even prevent bacterial adhesion, some bacterial anti-adhesion surface designs have been developed. However, the effect of some surface properties (including surface patterning, roughness and wettability) on bacterial adhesion has not been systematically summarized. In this review, a comprehensive overview of bacterial anti-adhesion surface design is presented. Modifying the surface pattern and roughness could reduce the contact area between bacteria and surfaces to weaken the initial adhesion force. Fabricating superhydrophobic surface or modifying hydrophilic functional groups could hinder the bacterial adhesion. The analysis and discussion about influencing factors of bacterial anti-adhesion surfaces provide basic guidelines on antibacterial surface design for future researches.
Cell-material interactions revealed via material techniques of surface patterning
[J].
Overview of hemostasis and thrombosis
[J].
Molecular markers of hemostasis: Introduction and overview
[J].
Oxidized regenerated cellulose/collagen dressings: Review of evidence and recommendations
[J].
Efficacy of oxidized regenerated cellulose/collagen dressing for management of skin wounds: A systematic review and meta-analysis
[J].
Study on cytotoxicity tests of medical devices based on IC50
[J].
基于IC50的医疗器械细胞毒性试验方法的研究
[J].
Cytotoxicity and its test methodology for a bioabsorbable nitrided iron stent
[J].
Improved biodegradable magnesium alloys through advanced solidification processing
[J].
Cytocompatibility evaluation of different biodegradable magnesium alloys with human mesenchymal stem cells
[J].
Endothelial cellular responses to biodegradable metal zinc
[J].Biodegradable zinc (Zn) metals, a new generation of biomaterials, have attracted much attention due to their excellent biodegradability, bioabsorbability, and adaptability to tissue regeneration. Compared with magnesium (Mg) and iron (Fe), Zn exhibits better corrosion and mechanical behaviors in orthopedic and stent applications. After implantation, Zn containing material will slowly degrade, and Zn ions (Zn) will be released to the surrounding tissue. For stent applications, the local Znconcentration near endothelial tissue/cells could be high. However, it is unclear how endothelia will respond to such high concentrations of Zn, which is pivotal to vascular remodeling and regeneration. Here, we evaluated the short-term cellular behaviors of primary human coronary artery endothelial cells (HCECs) exposed to a concentration gradient (0-140 μM) of extracellular Zn. Zn had an interesting biphasic effect on cell viability, proliferation, spreading, and migration. Generally, low concentrations of Zn promoted viability, proliferation, adhesion, and migration, while high concentrations of Zn had opposite effects. For gene expression profiles, the most affected functional genes were related to cell adhesion, cell injury, cell growth, angiogenesis, inflammation, vessel tone, and coagulation. These results provide helpful information and guidance for Zn-based alloy design as well as the controlled release of Znin stent and other related medical applications.
In vitro cytotoxicity, adhesion, and proliferation of human vascular cells exposed to zinc
[J].Zinc (Zn) and its alloys have recently been introduced as a new class of biodegradable metals with potential application in biodegradable vascular stents. Although an in vivo feasibility study pointed to outstanding biocompatibility of Zn-based implants in vascular environments, a thorough understanding of how Zn and Zn affect surrounding cells is lacking. In this comparative study, three vascular cell types-human endothelial cells (HAEC), human aortic smooth muscle cells (AoSMC), and human dermal fibroblasts (hDF)-were studied to advance the understanding of Zn/Zn-cell interactions. Aqueous cytotoxicity using a Zn insult assay resulted in LD values of 50 µM for hDF, 70 µM for AoSMC, and 265 µM for HAEC. Direct cell contact with the metallic Zn surface resulted initially in cell attachment, but was quickly followed by cell death. After modification of the Zn surface using a layer of gelatin-intended to mimic a protein layer seen in vivo-the cells were able to attach and proliferate on the Zn surface. Further experiments demonstrated a Zn dose-dependent effect on cell spreading and migration, suggesting that both adhesion and cell mobility may be hindered by free Zn.
Structure, mechanical characteristics and in vitro degradation, cytotoxicity, genotoxicity and mutagenicity of novel biodegradable Zn-Mg alloys
[J].
Influence of surface pre-treatment on the cytocompatibility of a novel biodegradable ZnMg alloy
[J].
The influence of alloying and fabrication techniques on the mechanical properties, biodegradability and biocompatibility of zinc: A comprehensive review
[J].Zinc has been identified as one of the most promising biodegradable metals along with magnesium and iron. Zinc appears to address some of the core engineering problems associated with magnesium and iron when applied to biomedical implant applications; hence the increase in the amount of research investigations on the metal in the last few years. In this review, the current state-of-the-art on biodegradable Zn, including recent developments, current opportunities and future directions of research are discussed. The discussions are presented with a specific focus on reviewing the relationships that exist between mechanical properties, biodegradability, and biocompatibility of zinc with alloying and fabrication techniques. This work hopes to guide future studies on biodegradable Zn that will help in advancing this field of research. STATEMENT OF SIGNIFICANCE: (i) The review offers an up-to-date and comprehensive review of the influence of alloying and fabrication technique on mechanical properties, biodegradability and biocompatibility of Zn; (ii) the work cites the most relevant biodegradable Zn fabrication processes including additive manufacturing techniques; (iii) the review includes a listing of research gap and future research directions for the field of biodegradable Zn.Copyright © 2019 Acta Materialia Inc. Published by Elsevier Ltd. All rights reserved.
Effects of Ag, Cu or Ca addition on microstructure and comprehensive properties of biodegradable Zn-0.8Mn alloy
[J].
Selection of extraction medium influences cytotoxicity of zinc and its alloys
[J].Zinc (Zn) alloys have been considered as promising absorbable metals, mainly due to their moderate degradation rates ranging between magnesium alloys and iron alloys. The degradation behavior depends on the specific physiological environment. Released metallic ions and corrosion products directly influence biocompatibility. The initial contact of orthopedic implants or vascular stents after implantation will be with blood. In this study, fetal bovine serum (FBS) was used as a model system of blood components. We investigated the influence of FBS on in vitro degradation behavior and cytotoxicity of pure Zn, and Zn-4Ag and Zn-2Ag-1.8Au-0.2 V (wt%) alloys. The initial degradation rates in FBS were assessed and compared with the degradation and toxicity in four other common physiological model systems: DMEM cell culture medium ± FBS and McCoy's 5A medium ± FBS. Test samples in pure FBS showed the highest initial degradation rates, and accordingly, FBS supplemented media accelerated the degradation process as well. Moreover, an extract test according to ISO 10993-5 and -12 with L929 and Saos-2 cells was performed to investigate the role of FBS in the extraction medium. The cytotoxic effects observed in the tests were correlated with FBS-mediated Zn release. These findings have significant implications regarding the selection of appropriate media for in vitro degradation and cytotoxicity evaluation of Zn and its alloys. STATEMENT OF SIGNIFICANCE: Metallic zinc and its alloys have been considered as promising biodegradable metals, mainly due to their moderate degradation rates. However, in vitro cytotoxicity tests according to the current ISO 10993 standard series are not suitable to predict biocompatibility of Zn alloys due to the inconsistent correlation between in vitro and in vitro biocompatibility. In this study, we show that the outcomes of standardized in vitro cytotoxicity tests of Zn and Zn alloys are influenced by fetal bovine serum in the extraction vehicle because FBS promotes Zn release during the extraction process. The results of the study provide significant information for selection of appropriate model systems to evaluate in vitro degradation behavior and cytotoxicity.Copyright © 2019 Acta Materialia Inc. Published by Elsevier Ltd. All rights reserved.
Zinc-based alloys for degradable vascular stent applications
[J].The search for biodegradable metals with mechanical properties equal or higher to those of currently used permanent biomaterials, such as stainless steels, cobalt chromium and titanium alloys, desirable in vivo degradation rate and uniform corrosion is still an open challenge. Magnesium (Mg), iron (Fe) and zinc (Zn)-based alloys have been proposed as biodegradable metals for medical applications. Over the last two decades, extensive research has been done on Mg and Fe. Fe-based alloys show appropriate mechanical properties, but their degradation rate is an order of magnitude below the benchmark value. In comparison, alongside the insufficient mechanical performance of most of its alloys, Mg degradation rate has proven to be too high in a physiological environment and corrosion is rarely uniform. During the last few years, Zn alloys have been explored by the biomedical community as potential materials for bioabsorbable vascular stents due to their tolerable corrosion rates and tunable mechanical properties. This review summarizes recent progress made in developing Zn alloys for vascular stenting application. Novel Zn alloys are discussed regarding their microstructural characteristics, mechanical properties, corrosion behavior and in vivo performance.Numerous studies on magnesium and iron materials have been reported to date, in an effort to formulate bioabsorbable stents with tailorable mechanical characteristics and corrosion behavior. Crucial concerns regarding poor ductility and remarkably rapid corrosion of magnesium, and very slow degradation of iron, seem to be still not desirably fulfilled. Zinc was introduced as a potential implant material in 2013 due to its promising biodegradability and biocompatibility. Since then, extensive investigations have been made toward development of zinc alloys that meet clinical benchmarks for vascular scaffolding. This review critically surveys the zinc alloys developed since 2013 from metallurgical and biodegradation points of view. Microstructural features, mechanical, corrosion and in vivo performances of these new alloys are thoroughly reviewed and evaluated.Copyright © 2018 Acta Materialia Inc. All rights reserved.
Recommendation for modifying current cytotoxicity testing standards for biodegradable magnesium-based materials
[J].As one of the most promising medical metal implants, magnesium (Mg) or its alloys have shown significant advantages over other candidates attributed to not only their excellent biodegradability and suitable mechanical properties but also their osteopromotive effects for bone applications. Prior to approval mandated by the governmental regulatory body, the access to the medical market for Mg-based implants requires a series of testing for assurance of their safety and efficacy via preclinical evaluations and clinical tests including phase 1 and 2 evaluations, and phase 3 of multi-center randomized double blind and placebo-controlled clinical trials. However, as the most widely used protocols for biosafety evaluation of medical devices, current ISO 10993 standards should be carefully reevaluated when directly applying them to predict potential health risks of degradable Mg based biomaterials via cytotoxicity tests due to the huge gap between in vitro and in vivo conditions. Therefore, instead of a direct adoption, modification of current ISO standards for in vitro cytotoxicity test is desirable and justified. The differences in sensitivities of cells to in vitro and in vivo Mg ions and the capability of in vivo circulation system to dilute local degradation products were fully considered to propose modification of current ISO standards. This paper recommended a minimal 6 times to a maximal 10 times dilution of extracts for in vitro cytotoxicity test specified in ISO 10993 part 5 for pure Mg developed as potential orthopedic implants based on literature review and our specifically designed in vitro and in vivo tests presented in the study. Our work may contribute to the progress of biodegradable metals involved translational work. Copyright © 2015 Acta Materialia Inc. Published by Elsevier Ltd. All rights reserved.
An overview of hemostasis
[J].Hemostasis is a remarkable and a remarkably complex mechanism. It can maintain blood in a fluid state intravascularly but very quickly changes blood to a jellylike mass upon disruption of the vasculature. This review will give a synopsis of the 3 phases of hemostasis: platelet, vascular, and coagulation. Fibrinolysis and control mechanisms of hemostasis will also be covered. In addition, brief descriptions of the clinical and laboratory evaluation of patients and the diagnosis of bleeding disorders will be presented.
Historical overview of the role of platelets in hemostasis and thrombosis
[J].Platelets were discovered by G. Bizzozero in 1882 and rediscovered in the 1960s after many decades of oblivion. Interestingly enough, their role was initially more clearly associated with thrombosis than with hemostasis. For many years a serious unresolved problem was that the clotting time was normal even in severe thrombocytopenia. The concept of coagulation as an enzymatic cascade had not yet been elaborated. During the 1960s, the interest of many experts moved from the interaction of platelets with the process of blood coagulation to the interaction of these cells with the vascular wall (adhesion) and each other (aggregation). The discovery of the role of ADP as the principle of platelet aggregation stimuli was rapidly followed by other important discoveries such as the aggregating properties of collagen and thrombin, the release reaction, the metabolism of arachidonic acid, and the inhibitory effect of aspirin. The use of aspirin as a potential antithrombotic drug has made the history of clinical trials in the last 30 years. The last two decades have been characterized by an explosion of cell and molecular biology approaches. There are presently people who study platelet signal transduction or platelet-leukocyte interactions but who know almost nothing about hemostasis or thrombosis! This is due not only to the intrinsic limitations of the biological approach but also to the progressive recognition of the role of platelets in other physiopathologic and clinical conditions such as inflammation, cancer growth and dissemination, and organ transplant rejection. Overlooked for more than two centuries after the microscope was made available to hematologists, considered as an artifact or a Cinderella, the platelet has mainly been considered in the past 30 years as a dangerous cell to be inhibited by (ever more expensive) drugs. But the taming of the shrew is far from being achieved.
Hemocompatibility of biodegradable Zn-0.8 wt% (Cu, Mn, Li) alloys
[J].
Micro-alloying with Mn in Zn-Mg alloy for future biodegradable metals application
[J].
Mechanical properties, in vitro degradation behavior, hemocompatibility and cytotoxicity evaluation of Zn-1.2Mg alloy for biodegradable implants
[J].
Microstructure, mechanical properties, in vitro degradation behavior and hemocompatibility of novel Zn-Mg-Sr alloys as biodegradable metals
[J].
Zinc exhibits ideal physiological corrosion behavior for bioabsorbable stents
[J].
Metallic zinc exhibits optimal biocompatibility for bioabsorbable endovascular stents
[J].
A simplified in vivo approach for evaluating the bioabsorbable behavior of candidate stent materials
[J].
Evolution of the degradation mechanism of pure zinc stent in the one-year study of rabbit abdominal aorta model
[J].In the present study, pure zinc stents were implanted into the abdominal aorta of rabbits for 12 months. Multiscale analysis including micro-CT, scanning electron microscopy (SEM), scanning transmission electron microscopy (STEM) and histological stainings was performed to reveal the fundamental degradation mechanism of the pure zinc stent and its biocompatibility. The pure zinc stent was able to maintain mechanical integrity for 6 months and degraded 41.75 ± 29.72% of stent volume after 12 months implantation. No severe inflammation, platelet aggregation, thrombosis formation or obvious intimal hyperplasia was observed at all time points after implantation. The degradation of the zinc stent played a beneficial role in the artery remodeling and healing process. The evolution of the degradation mechanism of pure zinc stents with time was revealed as follows: Before endothelialization, dynamic blood flow dominated the degradation of pure zinc stent, creating a uniform corrosion mode; After endothelialization, the degradation of pure zinc stent depended on the diffusion of water molecules, hydrophilic solutes and ions which led to localized corrosion. Zinc phosphate generated in blood flow transformed into zinc oxide and small amounts of calcium phosphate during the conversion of degradation microenvironment. The favorable physiological degradation behavior makes zinc a promising candidate for future stent applications.Copyright © 2017 Elsevier Ltd. All rights reserved.
Zn-Li alloy after extrusion and drawing: Structural, mechanical characterization, and biodegradation in abdominal aorta of rat
[J].
Novel high-strength, low-alloys Zn-Mg (< 0.1wt% Mg) and their arterial biodegradation
[J].
Evaluation of wrought Zn-Al alloys (1, 3, and 5 wt % Al) through mechanical and in vivo testing for stent applications
[J].
Inflammatory responses to biomaterials
[J].Implanted biomedical devices are of increasing importance in modern medical care. However, surprisingly little is known of the factors that determine biocompatibility of the materials used in these devices. These materials, although generally inert and non-toxic, can mediate a variety of adverse reactions, including inflammation, fibrosis, coagulation, and infection. This brief review focuses on the inflammatory responses (including fibrosis) that commonly occur around implanted biomaterials. Host proteins that spontaneously associate with implant surfaces are important determinants of the acute inflammatory response. In this regard, adsorbed fibrinogen appears particularly pro-inflammatory. Chronic inflammatory processes, in many cases in response to fragments of implanted biomaterials, may cause implant failure. In the case of silicone-filled mammary prostheses, the extravasation of silicone gel has been held responsible for a number of complications, including silicone granuloma, synovitis, connective-tissue disease, and lymphadenopathy. In some instances, material-mediated inflammatory responses may even cause degradation of the material itself (via oxidative products released by implant-associated inflammatory cells). Overall, there is insufficient knowledge of the determinants and mechanisms of host: implant responses. A clear understanding of tissue:biomaterial interactions will be required both to explain the pathogenesis of many implant-mediated complications and to aid in the development of more biocompatible materials for implantable devices.
Lumen gain and restoration of pulsatility after implantation of a bioresorbable vascular scaffold in porcine coronary arteries
[J].
Long-term in vivo study of biodegradable Zn-Cu stent: A 2-year implantation evaluation in porcine coronary artery
[J].In the present study, a novel biodegradable Zn-0.8Cu coronary artery stent was fabricated and implanted into porcine coronary arteries for up to 24 months. Micro-CT analysis showed that the implanted stent was able to maintain structural integrity after 6 months, while its disintegration occurred after 9 months of implantation. After 24 months of implantation, approximately 28 ± 13 vol% of the stent remained. Optical coherence tomography and histological analysis showed that the endothelialization process could be completed within the first month after implantation, and no inflammation responses or thrombosis formation was observed within 24 months. Cross-section analysis indicated that the subsequent degradation products had been removed in the abluminal direction, guaranteeing that the strut could be replaced by normal tissue without the risk of contaminating the circulatory system, causing neither thrombosis nor inflammation response. The present work demonstrates that the Zn-0.8Cu stent has provided sufficient structural supporting and exhibited an appropriate degradation rate during 24 months of implantation without degradation product accumulation, thrombosis, or inflammation response. The results indicate that the Zn-0.8Cu coronary artery stent is promising for further clinical applications. STATEMENT OF SIGNIFICANCE: Although Zn and its alloys have been considered to be potential candidates of biodegradable metals for vascular stent use, by far, no Zn-based stent with appropriate medical device performance has been reported because of the low mechanical properties of zinc. The present work presents promising results of a Zn-Cu biodegradable vascular stent in porcine coronary arteries. The Zn-Cu stent fabricated in this work demonstrated adequate medical device performance both in vitro and in vivo and degraded at a proper rate without safety problems induced. Furthermore, large animal models have more cardiovascular similarities as humans. Results of this study may provide further information of the Zn-based stents for translational medicine research.Copyright © 2019 Acta Materialia Inc. Published by Elsevier Ltd. All rights reserved.
Analysis of vascular inflammation against bioresorbable Zn-Ag-based alloys
[J].
Long-term surveillance of zinc implant in murine artery: Surprisingly steady biocorrosion rate
[J].Metallic zinc implanted into the abdominal aorta of rats out to 6months has been demonstrated to degrade while avoiding responses commonly associated with the restenosis of vascular implants. However, major questions remain regarding whether a zinc implant would ultimately passivate through the production of stable corrosion products or via a cell mediated fibrous encapsulation process that prevents the diffusion of critical reactants and products at the metal surface. Here, we have conducted clinically relevant long term in vivo studies in order to characterize late stage zinc implant biocorrosion behavior and products to address these critical questions. We found that zinc wires implanted in the murine artery exhibit steady corrosion without local toxicity for up to at least 20months post-implantation, despite a steady buildup of passivating corrosion products and intense fibrous encapsulation of the wire. Although fibrous encapsulation was not able to prevent continued implant corrosion, it may be related to the reduced chronic inflammation observed between 10 and 20months post-implantation. X-ray elemental and infrared spectroscopy analyses confirmed zinc oxide, zinc carbonate, and zinc phosphate as the main components of corrosion products surrounding the Zn implant. These products coincide with stable phases concluded from Pourbaix diagrams of a physiological solution and in vitro electrochemical impedance tests. The results support earlier predictions that zinc stents could become successfully bio-integrated into the arterial environment and safely degrade within a time frame of approximately 1-2years.Previous studies have shown zinc to be a promising candidate material for bioresorbable endovascular stenting applications. An outstanding question, however, is whether a zinc implant would ultimately passivate through the production of stable corrosion products or via a cell mediated tissue encapsulation process that prevented the diffusion of critical reactants and products at the metal surface. We found that zinc wires implanted in the murine artery exhibit steady corrosion for up to at least 20months post-implantation. The results confirm earlier predictions that zinc stents could safely degrade within a time frame of approximately 1-2years.Copyright © 2017 Acta Materialia Inc. Published by Elsevier Ltd. All rights reserved.
Zn-0.4Li alloy shows great potential for the fixation and healing of bone fractures at load-bearing sites
[J].
In vitro and in vivo studies of Zn-Mn biodegradable metals designed for orthopedic applications
[J].In recent years, Zn-based materials provide a new option as biodegradable metals for orthopedic applications. To improve the low strength and brittle nature of pure Zn, small amounts of alloying element Mn (0.1, 0.4 and 0.8 wt.%) were added into Zn to fabricate binary Zn-Mn alloys. An extremely high elongation (83.96 ± 2.36%) was achieved in the resulting Zn-0.8 wt.%Mn alloy. Moreover, Zn-Mn alloys displayed significantly improved cytocompatibility as compared to pure Zn, according to cell proliferation and morphology analyses. More importantly, a significantly improved osteogenic activity was verified after adding Mn regarding ALP activity and osteogenic expression. Furthermore, Zn-0.8 wt.%Mn alloy scaffolds were implanted into the rat femoral condyle for repairing bone defects with pure Ti as control. Enhanced osteogenic activities were confirmed for Zn-0.8Mn alloy in contrast to pure Ti based on Micro-CT and histological results, and favorable in vivo biosafety of Zn-0.8Mn alloy was verified by H&E staining and blood tests. The exceptional mechanical performance and favorable osteogenic capability render Zn-Mn alloy a promising candidate material in the treatment of bone defects or fracture repair. STATEMENT OF SIGNIFICANCE: The element Mn, on the one hand, as an essential trace element in the human body, promotes cell proliferation, adhesion, spreading, and regulates bone metabolism; on the other hand, it could significantly improve the ductility of Zn alloys. Here, we systematically reported the biocompatibility and biofunctionality of binary biodegradable Zn-Mn alloys in the bone environment. The Zn-Mn alloys promoted MC3T3-E1 cell proliferation, adhesion, spreading, and osteogenic differentiation in vitro. Furthermore, a rat femoral condyle defect model was established; porous Zn-Mn alloy scaffolds were manufactured to repair the bone defects. Significant bone regenerations, considerable bone ingrowth, and desirable biosafety were confirmed in vivo. Therefore, biodegradable Zn-Mn with promising osteogenic properties may become new options for orthopedic implant materials.Copyright © 2020. Published by Elsevier Ltd.
Biodegradable Zn-Sr alloy for bone regeneration in rat femoral condyle defect model: In vitro and in vivo studies
[J].Bone defects are commonly caused by severe trauma, malignant tumors, or congenital diseases and remain among the toughest clinical problems faced by orthopedic surgeons, especially when of critical size. Biodegradable zinc-based metals have recently gained popularity for their desirable biocompatibility, suitable degradation rate, and favorable osteogenesis-promoting properties. The biphasic activity of Sr promotes osteogenesis and inhibits osteoclastogenesis, which imparts Zn-Sr alloys with the ideal theoretical osteogenic properties. Herein, a biodegradable Zn-Sr binary alloy system was fabricated. The cytocompatibility and osteogenesis of the Zn-Sr alloys were significantly better than those of pure Zn in MC3T3-E1 cells. RNA-sequencing illustrated that the Zn-0.8Sr alloy promoted osteogenesis by activating the wnt/β-catenin, PI3K/Akt, and MAPK/Erk signaling pathways. Furthermore, rat femoral condyle defects were repaired using Zn-0.8Sr alloy scaffolds, with pure Ti as a control. The scaffold-bone integration and bone ingrowth confirmed the favorable in vivo repair properties of the Zn-Sr alloy, which was verified to offer satisfactory biosafety based on the hematoxylin-eosin (H&E) staining and ion concentration testing of important organs. The Zn-0.8Sr alloy was identified as an ideal bone repair material candidate, especially for application in critical-sized defects on load-bearing sites due to its favorable biocompatibility and osteogenic properties in vitro and in vivo.© 2020 [The Author/The Authors].
Ultrafine- and uniform-grained biodegradable Zn-0.5Mn alloy: Grain refinement mechanism, corrosion behavior, and biocompatibility in vivo
[J].
Alloying design of biodegradable zinc as promising bone implants for load-bearing applications
[J].Magnesium-based biodegradable metals (BMs) as bone implants have better mechanical properties than biodegradable polymers, yet their strength is roughly less than 350 MPa. In this work, binary Zn alloys with alloying elements Mg, Ca, Sr, Li, Mn, Fe, Cu, and Ag respectively, are screened systemically by in vitro and in vivo studies. Li exhibits the most effective strengthening role in Zn, followed by Mg. Alloying leads to accelerated degradation, but adequate mechanical integrity can be expected for Zn alloys when considering bone fracture healing. Adding elements Mg, Ca, Sr and Li into Zn can improve the cytocompatibility, osteogenesis, and osseointegration. Further optimization of the ternary Zn-Li alloy system results in Zn-0.8Li-0.4Mg alloy with the ultimate tensile strength 646.69 ± 12.79 MPa and Zn-0.8Li-0.8Mn alloy with elongation 103.27 ± 20%. In summary, biocompatible Zn-based BMs with strength close to pure Ti are promising candidates in orthopedics for load-bearing applications.
In vitro and in vivo studies of biodegradable Zn-Li-Mn alloy staples designed for gastrointestinal anastomosis
[J].Zn-0.8 wt.% Li-0.1 wt.% Mn wire with the diameter of 0.3 mm was fabricated and further processed into gastrointestinal staple, and its in vitro and in vivo biodegradation behavior and biocompatibility were studied systematically. The experimental Zn-Li-Mn alloy staple could deform from the original U-shape to B-shape without fracture, indicating its good mechanical property. Due to the residual stress concentration caused by anastomosis deformation, the feet and leg arc part of the staple were more prone to degradation. The Zn-Li-Mn alloy staple sustained integrity after immersion in Hanks' solution and simulated gastric fluid (SGF) for 28 days, and the degradation rate in SGF was about 4 times of that in Hanks' solution. Furthermore, Zn-Li-Mn alloy staples were utilized for gastrointestinal anastomosis in pig models, with clinically-used titanium alloy staples as a comparison. No anastomotic leakage and severe inflammation were observed after operation. The Zn-Li-Mn alloy staple maintained mechanical integrity within 8 weeks' implantation. The gastrointestinal tissue healed after 12 weeks, and no obvious side effects were detected during the whole implantation period, demonstrating the good biocompatibility of Zn-Li-Mn alloy staple. Thus, Zn-Li-Mn alloy staple fabricated in this work displayed the promising potential in the gastrointestinal anastomosis.Copyright © 2020. Published by Elsevier Ltd.
In vivo performances of pure Zn and Zn-Fe alloy as biodegradable implants
[J].
Biodegradable Zn-Cu alloys show antibacterial activity against MRSA bone infection by inhibiting pathogen adhesion and biofilm formation
[J].Bone and joint-related infections remain the primary and most critical complications of orthopedic surgery. We have innovatively prepared Zn-Cu alloys to achieve outstanding material and antibacterial properties. In this study, we systematically assessed the material properties and antibacterial activity of these Zn-Cu alloys. Our results showed that the Zn-2Cu alloy had the best mechanical properties, biocompatibility, and osteogenic properties. Findings of microbial cultures, CLSM, SEM, and TEM indicated that Zn-2Cu alloy can inhibit both coagulase-positive and coagulase-negative staphylococci, as well as antibiotic-resistant strains (MRSA and MRSE), by preventing the bacteria adhesion and the biofilm formation. Zn-2Cu alloy could broadly affect the expression of MRSA genes associated with adhesion, autolysis, biofilm formation, virulence, and drug resistance. A rat femur intramedullary nail infection-prevention model was established and the Zn-2Cu alloy-treated group showed significant antibacterial activity against MRSA and reduced the inflammatory toxic side-effects and infection-related bone loss. Collectively, our results indicate the potential utility of Zn-Cu alloy implants with 2 wt% Cu in treating orthopedic infections. Statement of significance: Osteomyelitis is a serious complication of orthopedic surgeries. Wide use of antibiotics contributes to the appearance of multi-drug resistant strains like methicillin-resistant staphylococcus aureus (MRSA). Alternatively, anti-osteomyelitis implants with broad-spectrum antibacterial properties can be favorable. Here, the antibacterial performance of biodegradable Zn-Cu alloys was evaluated with four different bacteria strains including antibiotic-resistant strains (MRSA and MRSE). Zn-Cu alloys exert excellent bacterial killing capability in all strains. In a rat femur infection model, the alloy showed significant antibacterial activity against MRSA and reduced inflammatory toxic side-effects as well as infection-related bone loss. The antibacterial property of Zn-2Cu alloy was associated with inhibition of gene expression related to wall synthesis, adhesion, colonization, biofilm formation, autolysis, and secretion of virulence factors in MRSA.Copyright © 2020. Published by Elsevier Ltd.
A biodegradable Zn-1Cu-0.1Ti alloy with antibacterial properties for orthopedic applications
[J].Zinc (Zn) alloys are receiving increasing attention in the field of biodegradable implant materials due to their unique combination of suitable biodegradability and good biological functionalities. However, the currently existing industrial Zn alloys are not necessarily biocompatible, nor sufficiently mechanically strong and wear-resistant. In this study, a Zn-1Cu-0.1Ti alloy is developed with enhanced mechanical strength, corrosion wear property, biocompatibility, and antibacterial ability for biodegradable implant material applications. HR and HR + CR were performed on the as-cast alloy and its microstructure, mechanical properties, frictional and wear behaviors, corrosion resistance, in vitro cytocompatibility, and antibacterial ability were systematically assessed. The microstructures of the Zn-1Cu-0.1Ti alloy after different deformation conditions included a η-Zn phase, a ε-CuZn phase, and an intermetallic phase of TiZn. The HR+CR sample of Zn-1Cu-0.1Ti exhibited a yield strength of 204.2 MPa, an ultimate tensile strength of 249.9 MPa, and an elongation of 75.2%; significantly higher than those of the HR alloy and the AC alloy. The degradation rate in Hanks' solution was 0.029 mm/y for the AC alloy, 0.032 mm/y for the HR+CR alloy, and 0.034 mm/y for the HR alloy. The HR Zn-1Cu-0.1Ti alloy showed the best wear resistance, followed by the AC alloy and the alloy after HR + CR. The extract of the AC Zn-1Cu-0.1Ti alloy showed over 80% cell viability with MC3T3-E1 pre-osteoblast and MG-63 osteosarcoma cells at a concentration of ≤ 25%. The as-cast Zn-1Cu-0.1Ti alloy showed good blood compatibility and antibacterial ability. STATEMENT OF SIGNIFICANCE: This work repots a Zn-1Cu-0.1Ti alloy with enhanced mechanical strength, corrosion wear property, biocompatibility, and antibacterial ability for biodegradable implant applications. Our findings showed that Zn-1Cu-0.1Ti after hot-rolling plus cold-rolling exhibited a yield strength of 204.2 MPa, an ultimate tensile strength of 249.9 MPa, an elongation of 75.2%, and a degradation rate of 0.032 mm/y in Hanks' Solution. The hot-rolled Zn-1Cu-0.1Ti showed the best wear resistance. The extract of the as-cast alloy at a concentration of ≤ 25% showed over 80% cell viability with MC3T3-E1 and MG-63 cells. The Zn-1Cu-0.1Ti alloy showed good hemocompatibility and antibacterial ability.Copyright © 2020. Published by Elsevier Ltd.
Systematical evolution on a Zn-Mg alloy potentially developed for biodegradable cardiovascular stents
[J].
Degradation behavior, cytotoxicity, hemolysis, and antibacterial properties of electro-deposited Zn-Cu metal foams as potential biodegradable bone implants
[J].Zinc (Zn) alloys have attracted much attention for biomedical applications due to their biodegradability, biocompatibility, and biological functionalities. Zn alloy foams have high potential to be used as regenerative medical implants by virtue of their porous structure, which allows new bone tissue ingrowth, their low elastic modulus approximating that of natural bone, and their biodegradation, which eliminates the need for follow-up surgery to remove the implants after bone tissue healing. In this context, a biodegradable Zn-Cu foam was fabricated by electrochemical deposition on a foamed Cu template and given a subsequent diffusion heat treatment. The microstructure, mechanical properties, degradation behavior, toxicity, hemolysis percentages, and antibacterial effects of the Zn-Cu foams were assessed for biomedical applications. The Zn-Cu foams exhibited a yield strength of ~12.1 MPa, a plateau strength of 16.8 MPa, and a strain over 50% under compression tests. The corrosion rate of the Zn-Cu foams measured by electrochemical polarization testing was 0.18 mm/y. The Zn-Cu foams showed good blood compatibility with a hemolysis percentage of less than 5%. Cytotoxicity assessment indicated that a 100% concentration of the Zn-Cu foam extract showed clear cytotoxicity against MC3T3-E1 osteoblast cells, but a 12.5% concentration of the extract showed > 90% cell viability. Moreover, the Zn-Cu foams showed good antibacterial effects. STATEMENT OF SIGNIFICANCE: This work reportsa biodegradable Zn-Cu foam with high mechanical strength and ductility, suitable degradation rate, good antibacterial capacity, and good hemolysis property and biocompatibility. The Zn-Cu foam exhibited a yield strength of ~12.1 MPa, a plateau strength of 16.8 MPa, and a strain over 50% under compression tests. The corrosion rate of the Zn-Cu foam measured by electrochemical polarization testing was 0.18 mm/y in Hanks' Solutions. The Zn-Cu foam showed good blood compatibility with a hemolysis percentage of less than 5%. Cytotoxicity assessment indicated that a 12.5% concentration of the foam extract showed > 90% cell viability. Moreover, the Zn-Cu foam showed good antibacterial effects against S. aureus.Copyright © 2019. Published by Elsevier Ltd.
Shifting focus from bacteria to host neutrophil extracellular traps of biodegradable pure Zn to combat implant centered infection
[J].The widespread use of orthopedic implants to support or replace bones is increasingly threatened by the risk of incurable bacterial infections, impenetrable microbial biofilms, and irreversible antibiotic resistance. In the past, the development of anti-infective biomaterials focused solely on direct antibacterial properties while ignoring the host's immune response. Inspired by the clearance of infection by the innate neutrophil response and participation in anti-infectious immunity of Zn ions, we report an innovative neutrophil extracellular traps (NETs) strategy, induced by biodegradable pure Zn, which achieved therapeutic efficacy toward biomaterial-related infections. Our and data showed that pure Zn was favorable for NETs formation by promoting the release of DNA fibers and granule proteins in a reactive oxygen species (ROS)-dependent manner, thereby retraining and degrading bacteria with an efficiency of up to 99.5%. Transcriptome analysis revealed that cytoskeletal rearrangement and toll-like receptor (TLR) signaling pathway were also involved in Zn-induced NETs formation. Furthermore, the results of a ()-infected rat model verified that pure Zn potentiated the bactericidal capability of neutrophils around implants, and promoted osseointegration in -infected rat femurs. This antibacterial immunity concept lays a foundation for the development of other antibacterial biomaterials and holds great promise for treating orthopedic infections.© 2022 The Authors.